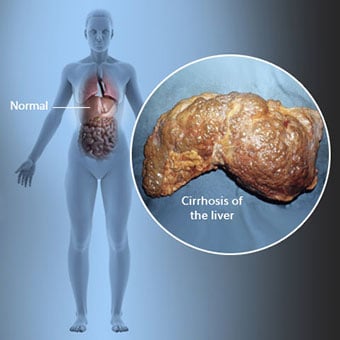
 Zirrhose ass eng Komplikatioun vun der Lebererkrankheet, déi Verloscht vun Liewerzellen an irreversibel Narben vun der Liewer involvéiert.
Zirrhose ass eng Komplikatioun vun der Lebererkrankheet, déi Verloscht vun Liewerzellen an irreversibel Narben vun der Liewer involvéiert. Leit mat Zirrhose kënne wéineg oder guer keng Symptomer an Zeeche vun der Lebererkrankheet hunn. E puer vun de Symptomer kënnen net spezifesch sinn, dat heescht, se proposéieren net datt d'Liewer hir Ursaach ass. E puer vun de méi heefegste Symptomer an Zeeche vun der Zirrhose enthalen:
Individuell mat Zirrhose entwéckelen och Symptomer an Zeeche vun de Komplikatioune vun der Zirrhose.
 Et gi vill Ursaache vun der Zirrhose abegraff Chemikalien (wéi Alkohol, Fett a bestëmmte Medikamenter), Viren, gëfteg Metaller, an Autoimmun Lebererkrankheet, an där den Immunsystem vum Kierper d'Liewer attackéiert.
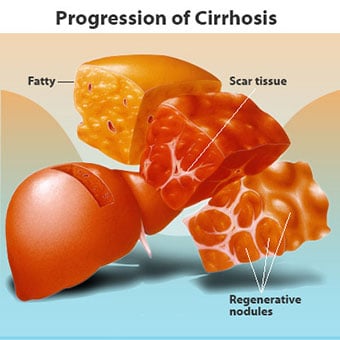
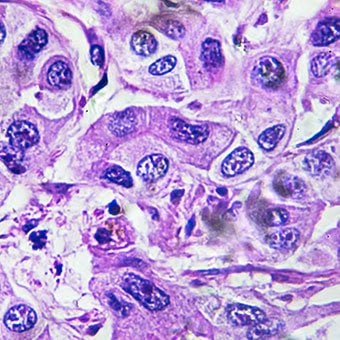
Et gi vill Ursaache vun der Zirrhose abegraff Chemikalien (wéi Alkohol, Fett a bestëmmte Medikamenter), Viren, gëfteg Metaller, an Autoimmun Lebererkrankheet, an där den Immunsystem vum Kierper d'Liewer attackéiert. Zirrhose ass eng Komplikatioun vu ville Lebererkrankheeten, charakteriséiert duerch anormal Struktur a Funktioun vun der Liewer. D'Krankheeten, déi zu Zirrhose féieren, maachen dat well se d'Leberzellen verletzen an ëmbréngen, duerno d'Entzündung an d'Reparatur, déi mat de stierwende Liewerzellen assoziéiert ass, Narbegewebe bilden. D'Liewerzellen déi net stierwen multiplizéieren an engem Versuch d'Zellen ze ersetzen déi gestuerwen sinn. Dëst resultéiert zu Stärekéip vun nei geformte Liewerzellen (regenerativ Knollen) am Narbengewebe. Et gi vill Ursaachen vun der Zirrhose, dorënner Chemikalien (wéi Alkohol, Fett a bestëmmte Medikamenter), Viren, gëfteg Metaller (wéi Eisen a Kupfer, déi an der Liewer accumuléieren als Resultat vun genetesche Krankheeten), an Autoimmun Liewer Krankheet den Immunsystem vum Kierper attackéiert d'Liewer.
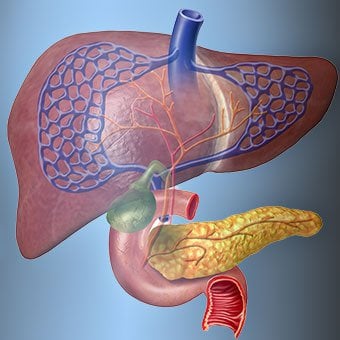
 D'Relatioun vun der Liewer zum Blutt ass eenzegaarteg.
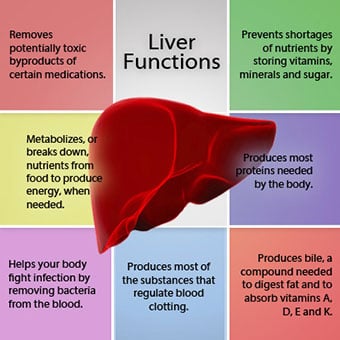
D'Relatioun vun der Liewer zum Blutt ass eenzegaarteg. D'Liewer ass e wichtegt Organ am Kierper. Et mécht vill kritesch Funktiounen aus, vun deenen zwee Substanzen produzéieren, déi vum Kierper erfuerderlech sinn, zum Beispill, clotting Proteinen, déi néideg sinn fir Blutt ze clotéieren, an d'Ewechhuele vu gëftege Substanzen, déi dem Kierper schiedlech kënne sinn, zum Beispill, wéi Drogen . D'Liewer spillt och eng wichteg Roll bei der Reguléierung vun der Versuergung vu Glukos (Zocker) a Lipiden (Fett), déi de Kierper als Brennstoff benotzt. Fir dës kritesch Funktiounen auszeféieren, mussen d'Leberzellen normal funktionnéieren, a si mussen eng Noperschaft zum Blutt hunn, well d'Substanzen, déi vun der Liewer dobäigesat oder ewechgeholl ginn, duerch d'Blutt an d'Liewer transportéiert ginn.
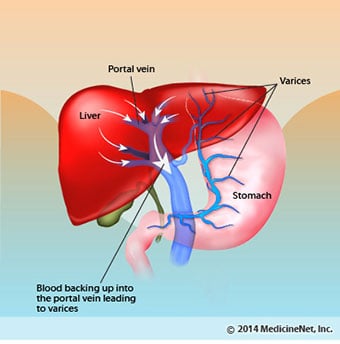
D'Relatioun vun der Liewer zum Blutt ass eenzegaarteg. Am Géigesaz zu de meescht Organer am Kierper gëtt nëmmen eng kleng Quantitéit u Blutt duerch Arterien an d'Liewer geliwwert. Déi meescht vun der Liewer Versuergung vu Blutt kënnt aus den Darm-Venen wéi d'Blutt an d'Häerz zréckkënnt. D'Haaptven, déi Blutt aus den Darm zréckkënnt, gëtt d'Portalven genannt. Wéi d'Portal Vene duerch d'Liewer passéiert, brécht se an ëmmer méi kleng a méi kleng Venen op. Déi klengst Venen (genannt Sinusoiden wéinst hirer eenzegaarteger Struktur) sinn am enke Kontakt mat den Liewerzellen. Liewerzellen riicht sech laanscht d'Längt vun de Sinusoiden. Dës enk Bezéiung tëscht den Liewerzellen a Blutt aus der Portalven erlaabt d'Leberzellen d'Substanzen an d'Blutt ze läschen. Wann d'Blutt duerch d'Sinusoiden passéiert ass, gëtt et an ëmmer méi grouss a méi grouss Venen gesammelt, déi schlussendlech eng eenzeg Ven bilden, d'Leberven, déi d'Blutt an d'Häerz zréckginn.
Bei Zirrhose gëtt d'Relatioun tëscht Blutt a Liewerzellen zerstéiert. Och wann d'Leberzellen, déi iwwerliewen oder nei geformt sinn, fäeg sinn Substanzen aus dem Blutt ze produzéieren an ze entfernen, hunn se net déi normal, intim Relatioun mam Blutt, an dat stéiert d'Fäegkeet vun den Liewerzellen fir Substanzen ze addéieren oder ze läschen. vum Blutt. Zousätzlech blockéiert d'Narben an der cirrhotescher Liewer de Bluttfluss duerch d'Liewer an d'Leberzellen. Als Resultat vun der Verhënnerung vum Bluttfluss duerch d'Liewer, "backup" Blutt an der Portalven, an den Drock an der Portalven eropgeet, eng Bedingung déi Portal Hypertonie genannt gëtt. Wéinst der Behënnerung vum Floss an héijen Drock an der Portalven, sicht Blutt an der Portalven aner Venen, an deenen se an d'Häerz zréckkommen, Venen mat nidderegen Drock, déi d'Liewer ëmgoen. Leider ass d'Liewer net fäeg Substanzen aus Blutt ze addéieren oder ze läschen, déi et ëmgoen. Et ass eng Kombinatioun vu reduzéierter Zuel vun Liewerzellen, Verloscht vum normale Kontakt tëscht Blutt, dat duerch d'Liewer an d'Liewerzellen passéiert, a Blutt, dat d'Liewer ëmgeet, wat zu villen Zeeche vun der Zirrhose féiert.
En zweete Grond fir d'Problemer vun der Zirrhose ass déi gestéiert Relatioun tëscht den Liewerzellen an de Kanäl, duerch déi d'Galle fléisst. Bile ass eng Flëssegkeet, déi vu Liewerzellen produzéiert gëtt, déi zwou wichteg Funktiounen huet:Hëllef bei der Verdauung an fir gëfteg Substanzen aus dem Kierper ze entfernen an ze eliminéieren. D'Galle produzéiert vu Liewerzellen gëtt a ganz kleng Kanäl ausgezeechent, déi tëscht den Liewerzellen lafen, déi d'Sinusoiden ausléisen, genannt Canaliculi. D'Canaliculi leien sech a kleng Kanäl aus, déi sech dann zesumme verbannen, fir ëmmer méi grouss Kanäl ze bilden. All d'Kanale kombinéieren an een Kanal deen an den Dënndarm kënnt, wou et mat der Verdauung vu Liewensmëttel hëllefe kann. Zur selwechter Zäit ginn gëfteg Substanzen, déi an der Galle enthale sinn, an den Darm an dann an den Hocker eliminéiert. Bei Zirrhose sinn d'Canaliculi anormal an d'Relatioun tëscht Liewerzellen a Canaliculi gëtt zerstéiert, grad wéi d'Relatioun tëscht den Liewerzellen a Blutt an de Sinusoiden. Als Resultat ass d'Liewer net fäeg gëfteg Substanzen normalerweis ze eliminéieren, a si kënnen am Kierper accumuléieren. Zu engem klengen Ausmooss gëtt d'Verdauung am Darm och reduzéiert.
 Allgemeng Symptomer an Zeeche vun der Zirrhose enthalen Geel, Middegkeet, Schwächt, Appetitverloscht, Jucken, an einfache Plooschteren.
Allgemeng Symptomer an Zeeche vun der Zirrhose enthalen Geel, Middegkeet, Schwächt, Appetitverloscht, Jucken, an einfache Plooschteren. Leit mat Zirrhose kënne wéineg oder guer keng Symptomer an Zeeche vun der Lebererkrankheet hunn. E puer vun de Symptomer kënnen net spezifesch sinn a proposéiere net datt d'Liewer hir Ursaach ass. Allgemeng Symptomer an Zeeche vun der Zirrhose enthalen:
Leit mat Zirrhose Wann d'Liewer och Symptomer an Zeeche vun de Komplikatioune vun der Krankheet entwéckelen.
Zirrhose u sech ass schonn e spéide Stadium vum Leberschued. An de fréie Stadien vun der Lebererkrankheet gëtt et Entzündung vun der Liewer. Wann dës Entzündung net behandelt gëtt, kann et zu Narbenbildung (Fibrose) féieren. Op dëser Etapp ass et nach ëmmer méiglech fir d'Liewer mat der Behandlung ze heelen.
Wann Fibrose vun der Liewer net behandelt gëtt, kann et zu Zirrhose féieren. Op dëser Etapp kann d'Narbengewebe net heelen, awer de Fortschrëtt vun der Narben kann verhënnert oder verlangsamt ginn. Leit mat Zirrhose, déi Zeeche vu Komplikatiounen hunn, kënnen Endstadium Lebererkrankheet (ESLD) entwéckelen an déi eenzeg Behandlung op dëser Etapp ass d'Lebertransplantatioun.
 Ödem, Ascites a bakteriell Peritonitis Komplikatiounen
Ödem, Ascites a bakteriell Peritonitis Komplikatiounen Wéi d'Zirrhose vun der Liewer schwéier gëtt, ginn Signaler an d'Niere geschéckt fir Salz a Waasser am Kierper ze halen. D'iwwerschësseg Salz a Waasser accumuléiert als éischt am Tissu ënner der Haut vun de Knöchel a Been wéinst dem Effekt vun der Schwéierkraaft beim Stand oder beim Sëtzen. Dës Akkumulation vu Flëssegkeet gëtt periphere Ödem oder Pittingödem genannt. (Pitting edema bezitt sech op d'Tatsaach, datt e Fangerspëtzt fest géint e Knöchel oder Been mat Ödem dréckt, verursaacht eng Abriecherung an der Haut, déi eng Zäit no der Verëffentlechung vum Drock bestoe bleift. All Typ vun Drock, wéi z. , kann genuch sinn fir Pitting ze verursaachen.) D'Schwellung ass dacks méi schlëmm um Enn vun engem Dag nodeems se stoen oder sëtzen a kënnen iwwer Nuecht erofgoen wann Dir leet. Wéi d'Zirrhose verschlechtert a méi Salz a Waasser zréckbehale ginn, kann Flëssegkeet och an der Bauchhöhle tëscht der Bauchmauer an de Bauchorganer (Ascites genannt) accumuléieren, wat Schwellung vum Bauch, Bauchbehënnerung a méi Gewiicht verursaacht.
Flëssegkeet am Bauchhöhl (Ascites) ass déi perfekt Plaz fir Bakterien ze wuessen. Normalerweis enthält de Bauchhöhl eng ganz kleng Quantitéit vu Flëssegkeet, déi d'Infektioun gutt widderstoen kann, a Bakterien, déi an de Bauch erakommen (normalerweis aus dem Darm) ginn ëmbruecht oder fannen de Wee an d'Portal-Ven an an d'Liewer, wou se ëmbruecht ginn. Bei Zirrhose ass d'Flëssegkeet, déi am Bauch sammelt, net fäeg fir d'Infektioun normalerweis ze widderstoen. Ausserdeem fanne méi Bakterien de Wee vum Darm an d'Ascites. D'Infektioun am Bauch an den Ascites, genannt spontan bakteriell Peritonitis oder SBP, ass méiglecherweis optrieden. SBP ass eng liewensgeféierlech Komplikatioun. E puer Patienten mat SBP hu keng Symptomer, anerer hunn Féiwer, Rillen, Bauchschmerzen an Zärtheet, Diarrho a verschlechtert Ascites.
 Komplikatioune vu Blutungen a Milz
Komplikatioune vu Blutungen a Milz An der cirrhotescher Liewer blockéiert d'Narbengewebe de Bluttfluss, deen aus den Darm an d'Häerz zréckkënnt an erhéicht den Drock an der Portalven (Portal Hypertonie). Wann den Drock an der Portalven héich genuch gëtt, féiert dat Blutt ronderëm d'Liewer duerch Venen mat nidderegen Drock fir d'Häerz z'erreechen. Déi heefegst Venen, duerch déi d'Blutt d'Liewer ëmgeet, sinn d'Venen, déi den ënneschten Deel vun der Speiseröh an den ieweschten Deel vum Magen bedeckt.
Als Resultat vun der verstäerkter Flux vum Blutt an der doraus resultéierend Erhéijung vun Drock, d'Venen an der ënneschter esophagus an ieweschte Mo expandéieren an dann als esophageal an gastric Varizen bezeechent; wat méi héich de Portal Drock ass, wat d'Varizen méi grouss sinn an dest méi wahrscheinlech ass e Patient aus de Varizen an d'Speiseröhre oder de Mo ze blutt.
Blutungen aus Varizen ass schwéier an ouni direkt Behandlung kann fatal sinn. Symptomer vu Blutungen aus Varizen enthalen Blutt Erbrechung (et ka schéngen als rout Blutt gemëscht mat Knollen oder "Kaffisgrënn"), Stool passéiert deen schwaarz a tarry ass wéinst Verännerungen am Blutt wéi et duerch den Darm passéiert (melena), an orthostatesch. Schwindel oder Schwindel (verursaacht duerch eng Ofsenkung vum Blutdrock, besonnesch wann Dir aus enger lieger Positioun opstinn).
Blutungen kënnen selten aus Varizen optrieden, déi soss anzwousch am Darm bilden, zum Beispill de Colon. Patienten, déi hospitaliséiert sinn wéinst aktiv Blutungen vun der Speiseröhre Varizen hunn e grousse Risiko fir spontan bakteriell Peritonitis z'entwéckelen, obwuel d'Grënn dofir nach net verstanen sinn.
D'Milz wierkt normalerweis als Filter fir eeler rout Bluttzellen, wäiss Bluttzellen a Plättchen ze entfernen (kleng Partikele wichteg fir d'Stammung vum Blutt.). D'Blutt, dat aus der Mëlz ofleeft, schléisst d'Blutt an d'Portalven aus den Darm. Wéi den Drock an der Portalven an der Zirrhose eropgeet, blockéiert et ëmmer méi de Bluttfluss aus der Milz. D'Blutt "back-up", accumuléiert an der Milz, an d'Milz schwëllt an der Gréisst, eng Bedingung déi als Splenomegalie bezeechent gëtt. Heiansdo ass d'Milz sou vergréissert datt et Bauchschmerzen verursaacht.
Wéi d'Mëlz vergréissert, filtert se ëmmer méi vun de Bluttzellen a Plaquetten aus, bis hir Zuel am Blutt reduzéiert gëtt. Hypersplenism ass de Begrëff, dee benotzt gëtt fir dës Bedingung ze beschreiwen, an et ass verbonne mat engem nidderegen rout Bluttzellzuel (Anämie), gerénger wäiss Bluttzellzuel (Leukopenie), an / oder engem nidderegen Thrombozytopenie (Thrombozytopenie). Anämie kann Schwächt verursaachen, Leukopenie kann zu Infektiounen féieren, an Thrombozytopenie kann d'Bluttgerinnung beeinträchtigen an zu längerer Blutungen féieren
 Liewer (hepatesch) Komplikatiounen
Liewer (hepatesch) Komplikatiounen Zirrhose wéinst all Ursaach erhéicht de Risiko vu primäre Liewerkriibs (hepatozellulär Karzinom). Primär bezitt sech op d'Tatsaach datt den Tumor an der Liewer staamt. E sekundäre Liewerkriibs ass een deen soss anzwousch am Kierper entstinn a sech an d'Liewer verbreet (metastaséiert).
Déi heefegst Symptomer an Unzeeche vum primäre Lebererkrank sinn Bauchschmerzen a Schwellungen, eng vergréissert Liewer, Gewiichtsverloscht a Féiwer. Zousätzlech kënnen Lebererkrankheeten eng Rei vu Substanzen produzéieren an entloossen, dorënner déi, déi eng Erhéijung vun der Zuel vu roude Bluttzellen (erythrozytose), nidderegen Bluttzocker (Hypoglykämie) an héije Bluttkalzium (Hyperkalzämie) verursaachen.
E puer vun de Proteinen a Liewensmëttel, déi d'Verdauung an d'Absorptioun entkommen, gëtt vu Bakterien benotzt, déi normalerweis am Darm präsent sinn. Wärend de Protein fir hir eegen Zwecker benotzt, maachen d'Bakterien Substanzen, déi se an den Darm entloossen, fir dann an de Kierper absorbéiert ze ginn. E puer vun dëse Substanzen, wéi Ammoniak, kënnen gëfteg Auswierkungen op d'Gehir hunn. Normalerweis ginn dës gëfteg Substanzen aus dem Darm an der Portalven an d'Liewer gedroen, wou se aus dem Blutt erausgeholl an entgëfteg ginn.
Wann Zirrhose präsent ass, kënnen d'Leberzellen net normal funktionnéieren entweder well se beschiedegt sinn oder well se hir normal Relatioun mam Blutt verluer hunn. Zousätzlech ass e puer Blutt an der Portalvene d'Liewer duerch aner Venen ëmgaang. D'Resultat vun dësen Anomalie ass datt gëfteg Substanzen net vun den Liewerzellen ewechgeholl kënne ginn, an amplaz am Blutt accumuléieren.
Wann déi gëfteg Substanzen genuch am Blutt accumuléieren, gëtt d'Funktioun vum Gehir behënnert, eng Bedingung déi hepatesch Ensephalopathie genannt gëtt. Schlof am Dag anstatt an der Nuecht (Reversatioun vum normale Schlofmuster) ass e fréie Symptom vun der hepatescher Ensephalopathie. Aner Symptomer enthalen Reizbarkeet, Onméiglechkeet sech ze konzentréieren oder Berechnungen ze maachen, Erënnerungsverloscht, Duercherneen oder depriméiert Bewosstsinnsniveauen. Schliisslech verursaacht schwéier Hepatesch Ensephalopathie Koma an Doud.
Déi gëfteg Substanzen maachen och d'Gehirer vu Patienten mat Zirrhose ganz empfindlech fir Medikamenter déi normalerweis vun der Liewer gefiltert an entgëfteg sinn. Dosen vu villen Drogen musse vläicht reduzéiert ginn fir eng gëfteg Opbau an der Zirrhose ze vermeiden, besonnesch Berouegungsmëttel an Drogen déi benotzt gi fir de Schlof ze förderen. Alternativ kënnen Drogen benotzt ginn, déi net mussen entgëften oder aus dem Kierper duerch d'Liewer eliminéiert ginn, wéi Drogen, déi vun den Nieren eliminéiert ginn.
Patienten mat verschlechtert Zirrhose kënnen hepatorenal Syndrom entwéckelen. Dëst Syndrom ass eng sérieux Komplikatioun an där d'Funktioun vun den Nieren reduzéiert gëtt. Et ass e funktionnelle Problem an den Nieren, dat heescht datt et kee kierperleche Schued un den Nieren ass. Amplaz ass déi reduzéiert Funktioun wéinst Verännerungen an der Art a Weis wéi d'Blutt duerch d'Nier selwer fléisst. Den hepatorenalen Syndrom ass definéiert als progressiv Versoen vun den Nieren fir Substanzen aus dem Blutt ze läschen an adäquate Quantitéiten un Urin ze produzéieren, während aner wichteg Funktioune vun der Nier, wéi d'Retentioun vu Salz, erhale bleiwen. Wann d'Leberfunktioun verbessert oder eng gesond Liewer an e Patient mat hepatorenalen Syndrom transplantéiert gëtt, fänken d'Nieren normalerweis erëm normal ze schaffen. Dëst hindeit datt d'reduzéiert Funktioun vun den Nieren d'Resultat ass entweder vun der Akkumulation vun gëftege Substanzen am Blutt oder enger anormaler Leberfunktioun wann d'Liewer fällt. Et ginn zwou Aarte vum hepatorenalen Syndrom. Eng Zort geschitt graduell iwwer Méint. Déi aner geschitt séier iwwer eng Woch oder zwou.
Selten, e puer Patienten mat fortgeschratt cirrhosis kënnen hepatopulmonary Syndrom entwéckelen. Dës Patienten kënnen Atmungsschwieregkeeten erliewen, well verschidde Hormonen, déi an der fortgeschratter Zirrhose verëffentlecht ginn, d'Lunge verursaachen anormal funktionnéieren. De Basisproblem an der Lunge ass datt net genuch Blutt duerch déi kleng Bluttgefässer an de Lunge fléisst, déi a Kontakt mat den Alveoli (Loftsäck) vun de Lunge sinn. Blutt dat duerch d'Lunge fléisst gëtt ronderëm d'Alveoli shunted a kann net genuch Sauerstoff aus der Loft an den Alveoli ophuelen. Als Resultat erlieft de Patient kuerz Atem, besonnesch mat Ustrengung.
 Et ginn 12 allgemeng Ursaachen vun der Zirrhose.
Et ginn 12 allgemeng Ursaachen vun der Zirrhose. Allgemeng Ursaachen vun der Liewerzirrhose enthalen:
Manner allgemeng Ursaachen vun Zirrhose enthalen:
A verschiddenen Deeler vun der Welt (besonnesch Nordafrika) ass d'Infektioun vun der Liewer mat engem Parasit (Schistosomiasis) déi heefegst Ursaach vun der Lebererkrankheet an der Zirrhose.
 Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis.
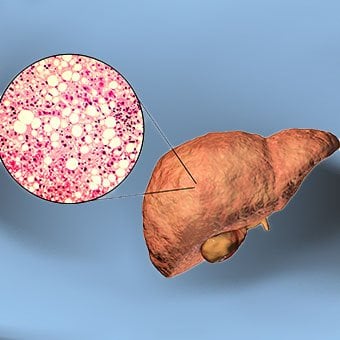
Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis. Alcohol is a very common cause of cirrhosis, particularly in the Western world. Chronic, high levels of alcohol consumption injure liver cells. Thirty percent of individuals who drink daily at least eight to sixteen ounces of hard liquor or the equivalent for fifteen or more years will develop cirrhosis. Alcohol causes a range of liver diseases, which include simple and uncomplicated fatty liver (steatosis), more serious fatty liver with inflammation (steatohepatitis or alcoholic hepatitis), and cirrhosis.
Nonalcoholic fatty liver disease (NAFLD) refers to a wide spectrum of liver diseases that, like alcoholic liver disease, range from simple steatosis, to nonalcoholic steatohepatitis (NASH), to cirrhosis. All stages of NAFLD have in common the accumulation of fat in liver cells. The term nonalcoholic is used because NAFLD occurs in individuals who do not consume excessive amounts of alcohol, yet in many respects the microscopic picture of NAFLD is similar to what can be seen in liver disease that is due to excessive alcohol. NAFLD is associated with a condition called insulin resistance, which, in turn, is associated with metabolic syndrome and diabetes mellitus type 2. Obesity is the main cause of insulin resistance, metabolic syndrome, and type 2 diabetes. NAFLD is the most common liver disease in the United States and is responsible for up to 25% of all liver disease. The number of livers transplanted for NAFLD-related cirrhosis is on the rise. Public health officials are worried that the current epidemic of obesity will dramatically increase the development of NAFLD and cirrhosis in the population.
 Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women.
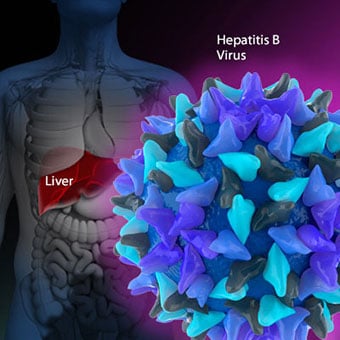
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. Chronic viral hepatitis is a condition in which hepatitis B or hepatitis C virus infects the liver for years. Most patients with viral hepatitis will not develop chronic hepatitis and cirrhosis. The majority of patients infected with hepatitis A recover completely within weeks, without developing chronic infection. In contrast, some patients infected with hepatitis B virus and most patients infected with hepatitis C virus develop chronic hepatitis, which, in turn, causes progressive liver damage and leads to cirrhosis, and, sometimes, liver cancers.
Autoimmune hepatitis is a liver disease found more commonly in women that is caused by an abnormality of the immune system. The abnormal immune activity in autoimmune hepatitis causes progressive inflammation and destruction of liver cells (hepatocytes), leading ultimately to cirrhosis.
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. The abnormal immunity in PBC causes chronic inflammation and destruction of the small bile ducts within the liver. The bile ducts are passages within the liver through which bile travels to the intestine. Bile is a fluid produced by the liver that contains substances required for digestion and absorption of fat in the intestine, as well as other compounds that are waste products, such as the pigment bilirubin. (Bilirubin is produced by the breakdown of hemoglobin from old red blood cells.). Along with the gallbladder, the bile ducts make up the biliary tract. In PBC, the destruction of the small bile ducts blocks the normal flow of bile into the intestine. As the inflammation continues to destroy more of the bile ducts, it also spreads to destroy nearby liver cells. As the destruction of the hepatocytes proceeds, scar tissue (fibrosis) forms and spreads throughout the areas of destruction. The combined effects of progressive inflammation, scarring, and the toxic effects of accumulating waste products culminates in cirrhosis.
Primary sclerosing cholangitis (PSC) is an uncommon disease frequently found in patients with Crohn's disease and ulcerative colitis. In PSC, the large bile ducts outside of the liver become inflamed, narrowed, and obstructed. Obstruction to the flow of bile leads to infections of the bile ducts and jaundice, eventually causing cirrhosis. In some patients, injury to the bile ducts (usually because of surgery) also can cause obstruction and cirrhosis of the liver.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. Inherited (genetic) disorders that result in the accumulation of toxic substances in the liver, which leads to tissue damage and cirrhosis. Examples include the abnormal accumulation of iron (hemochromatosis) or copper (Wilson disease). In hemochromatosis, patients inherit a tendency to absorb an excessive amount of iron from food. Over time, iron accumulation in different organs throughout the body causes cirrhosis, arthritis, heart muscle damage leading to heart failure, and testicular dysfunction causing loss of sexual drive. Treatment is aimed at preventing damage to organs by removing iron from the body through phlebotomy (removing blood). In Wilson disease, there is an inherited abnormality in one of the proteins that control copper in the body. Over time, copper accumulates in the liver, eyes, and brain. Cirrhosis, tremor, psychiatric disturbances, and other neurological difficulties occur if the condition is not treated early. Treatment is with oral medication, which increases the amount of copper that is eliminated from the body in the urine.
Cryptogenic cirrhosis (cirrhosis due to unidentified causes) is a common reason for liver transplantation. It is termed called cryptogenic cirrhosis because for many years doctors have been being unable to explain why a proportion of patients developed cirrhosis. Doctors now believe that cryptogenic cirrhosis is due to NASH (nonalcoholic steatohepatitis) caused by long-standing obesity, type 2 diabetes, and insulin resistance. The fat in the liver of patients with NASH is believed to disappear with the onset of cirrhosis, and this has made it difficult for doctors to make the connection between NASH and cryptogenic cirrhosis for a long time. One important clue that NASH leads to cryptogenic cirrhosis is the finding of a high occurrence of NASH in the new livers of patients undergoing liver transplant for cryptogenic cirrhosis. Finally, a study from France suggests that patients with NASH have a similar risk of developing cirrhosis as patients with long-standing infection with hepatitis C virus. (See discussion that follows.) However, the progression to cirrhosis from NASH is thought to be slow and the diagnosis of cirrhosis typically is made in people in their sixties.
Infants can be born without bile ducts (biliary atresia) and ultimately develop cirrhosis. Other infants are born lacking vital enzymes for controlling sugars that lead to the accumulation of sugars and cirrhosis. On rare occasions, the absence of a specific enzyme can cause cirrhosis and scarring of the lung (alpha-1 antitrypsin deficiency).
Less common causes of cirrhosis include unusual reactions to some drugs and prolonged exposure to toxins, as well as chronic heart failure (cardiac cirrhosis). In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. The single best test for diagnosing cirrhosis is a biopsy of the liver. Liver biopsies carry a small risk for serious complications, and biopsy often is reserved for those patients in whom the diagnosis of the type of liver disease or the presence of cirrhosis is not clear. The history, physical examination, or routine testing may suggest the possibility of cirrhosis. If cirrhosis is present, other tests can be used to determine the severity of the cirrhosis and the presence of complications. Tests also may be used to diagnose the underlying disease that is causing the cirrhosis. Examples of how doctors diagnose and evaluate cirrhosis are:
 There are four types of treatment of cirrhosis.
There are four types of treatment of cirrhosis. Treatment of cirrhosis includes
Consume a balanced diet and one multivitamin daily. Patients with PBC with impaired absorption of fat-soluble vitamins may need additional vitamins D and K.
Avoid drugs (including alcohol) that cause liver damage. All patients with cirrhosis should avoid alcohol. Most patients with alcohol-induced cirrhosis experience an improvement in liver function with abstinence from alcohol. Even patients with chronic hepatitis B and C can substantially reduce liver damage and slow the progression towards cirrhosis with abstinence from alcohol.
Avoid nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen). Patients with cirrhosis can experience worsening of liver and kidney function with NSAIDs.
Eradicate hepatitis B and hepatitis C virus by using anti-viral medications. Not all patients with cirrhosis due to chronic viral hepatitis are candidates for drug treatment. Some patients may experience serious deterioration in liver function and/or intolerable side effects during treatment. Thus, decisions to treat viral hepatitis have to be individualized, after consulting with doctors experienced in treating liver diseases (hepatologists).
Remove blood from patients with hemochromatosis to reduce the levels of iron and prevent further damage to the liver. In Wilson's disease, medications can be used to increase the excretion of copper in the urine to reduce the levels of copper in the body and prevent further damage to the liver.
Suppress the immune system with drugs such as prednisone and azathioprine (Imuran) to decrease inflammation of the liver in autoimmune hepatitis.
Treat patients with PBC with a bile acid preparation, ursodeoxycholic acid (UDCA), also called ursodiol (Actigall). Results of an analysis that combined the results from several clinical trials showed that UDCA increased survival among PBC patients during 4 years of therapy. The development of portal hypertension also was reduced by the UDCA. It is important to note that despite producing clear benefits, UDCA treatment primarily retards progression and does not cure PBC. Other medications such as colchicine and methotrexate also may have benefits in subsets of patients with PBC.
Immunize patients with cirrhosis against infection with hepatitis A and B to prevent a serious deterioration in liver. There are currently no vaccines available for immunizing against hepatitis C.
 Treatment for edema, ascites, and hypersplenism complications.
Treatment for edema, ascites, and hypersplenism complications. Retaining salt and water can lead to swelling of the ankles and legs (edema) or abdomen (ascites) in patients with cirrhosis. Doctors often advise patients with cirrhosis to restrict dietary salt (sodium) and fluid to decrease edema and ascites. The amount of salt in the diet usually is restricted to 2 grams per day and fluid to 1.2 liters per day. In most patients with cirrhosis, salt and fluid restriction is not enough and diuretics have to be added.
Diuretics are medications that work in the kidneys to promote the elimination of salt and water into the urine. A combination of the diuretics spironolactone (Aldactone) and furosemide (Lasix) can reduce or eliminate the edema and ascites in most patients. During treatment with diuretics, it is important to monitor the function of the kidneys by measuring blood levels of blood urea nitrogen (BUN) and creatinine to determine if too much diuretic is being used. Too much diuretic can lead to kidney dysfunction that is reflected in elevations of the BUN and creatinine levels in the blood.
Sometimes, when the diuretics do not work (in which case the ascites is said to be refractory), a long needle or catheter is used to draw out the ascitic fluid directly from the abdomen, a procedure called abdominal paracentesis. It is common to withdraw large amounts (liters) of fluid from the abdomen when the ascites is causing painful abdominal distension and/or difficulty breathing because it limits the movement of the diaphragms.
Another treatment for refractory ascites is a procedure called transjugular intravenous portosystemic shunting (TIPS).
The spleen normally acts as a filter to remove older red blood cells, white blood cells, and platelets (small particles important for the clotting of blood). The blood that drains from the spleen joins the blood in the portal vein from the intestines. As the pressure in the portal vein rises in cirrhosis, it increasingly blocks the flow of blood from the spleen. The blood "backs-up," accumulating in the spleen, and the spleen swells in size, a condition referred to as splenomegaly. Sometimes, the spleen is so enlarged it causes abdominal pain.
As the spleen enlarges, it filters out more and more of the blood cells and platelets until their numbers in the blood are reduced. Hypersplenism is the term used to describe this condition, and it is associated with a low red blood cell count (anemia), low white blood cell count (leukopenia), and/or a low platelet count (thrombocytopenia). Anemia can cause weakness, leucopenia can lead to infections, and thrombocytopenia can impair the clotting of blood and result in prolonged bleeding.
 Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding.
Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. If large varices develop in the esophagus or upper stomach, patients with cirrhosis are at risk for serious bleeding due to rupture of these varices. Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. Treatments include medications and procedures to decrease the pressure in the portal vein and procedures to destroy the varices.
 Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose.
Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Patients with an abnormal sleep cycle, impaired thinking, odd behavior, or other signs of hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Dietary protein is restricted because it is a source of toxic compounds that cause hepatic encephalopathy. Lactulose, which is a liquid, traps toxic compounds in the colon so they cannot be absorbed into the bloodstream, and thus cause encephalopathy. Lactulose is converted to lactic acid in the colon, and the acidic environment that results is believed to trap the toxic compounds produced by the bacteria. To be sure adequate lactulose is present in the colon at all times, the patient should adjust the dose to produce 2 to 3 semiformed bowel movements a day. Lactulose is a laxative, and the effectiveness of treatment can be judged by loosening or increasing the frequency of stools. Rifaximin (Xifaxan) is an antibiotic taken orally that is not absorbed into the body but rather remains in the intestines. It is the preferred mode of treatment of hepatic encephalopathy. Antibiotics work by suppressing the bacteria that produce the toxic compounds in the colon.
 Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics.
Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics. Patients suspected of having spontaneous bacterial peritonitis usually will undergo paracentesis. The fluid that is removed is examined for white blood cells and cultured for bacteria. Culturing involves inoculating a sample of the ascites into a bottle of nutrient-rich fluid that encourages the growth of bacteria, thus facilitating the identification of even small numbers of bacteria. Blood and urine samples also are often obtained for culturing because many patients with spontaneous bacterial peritonitis also will have infections in their blood and urine. Many doctors believe the infection may have begun in the blood and the urine and spread to the ascitic fluid to cause spontaneous bacterial peritonitis. Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics such as cefotaxime (Claforan). Patients usually treated with antibiotics include:
Spontaneous bacterial peritonitis is a serious infection. It often occurs in patients with advanced cirrhosis whose immune systems are weak, but with modern antibiotics and early detection and treatment, the prognosis of recovering from an episode of spontaneous bacterial peritonitis is good.
In some patients, oral antibiotics (norfloxacin [Noroxin] or sulfamethoxazole and trimethoprim [Bactrim]) can be prescribed to prevent spontaneous bacterial peritonitis. Not all patients with cirrhosis and ascites should be treated with antibiotics to prevent spontaneous bacterial peritonitis, but some patients are at high risk for developing spontaneous bacterial peritonitis and warrant preventive treatment.
 The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases. Several types of liver disease that cause cirrhosis (such as hepatitis B and C) are associated with a high incidence of liver cancer. It is useful to screen for liver cancer in patients with cirrhosis, as early surgical treatment or transplantation of the liver can cure the patient of cancer. The difficulty is that the methods available for screening are only partially effective, identifying at best only half of patients at a curable stage of their cancer. Despite the partial effectiveness of screening, most patients with cirrhosis, particularly hepatitis B and C, are screened yearly or every six months with ultrasound examination of the liver and measurements of cancer-produced proteins in the blood, for example, alpha-fetoprotein.
Cirrhosis is irreversible. Liver function usually gradually worsens despite treatment, and complications of cirrhosis increase and become difficult to treat. When cirrhosis is far advanced liver transplantation often is the only option for treatment. Recent advances in surgical transplantation and medications to prevent infection and rejection of the transplanted liver have greatly improved survival after transplantation. On average, more than 80% of patients who receive transplants are alive after five years. Not everyone with cirrhosis is a candidate for transplantation. Furthermore, there is a shortage of livers to transplant, and they're usually is a long (months to years) wait before a liver for transplanting becomes available. Measures to slow the progression of liver disease, and treat and prevent complications of cirrhosis are vitally important.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
Progress in the management and prevention of cirrhosis continues. Research is ongoing to determine the mechanism of scar formation in the liver and how this process of scarring can be interrupted or even reversed. Newer and better treatments for viral liver disease are being developed to prevent the progression to cirrhosis. Prevention of viral hepatitis by vaccination, which is available for hepatitis B, is being developed for hepatitis C. Treatments for the complications of cirrhosis are being developed or revised, and tested continually. Finally, research is being directed at identifying new proteins in the blood that can detect liver cancer early or predict which patients will develop liver cancer.
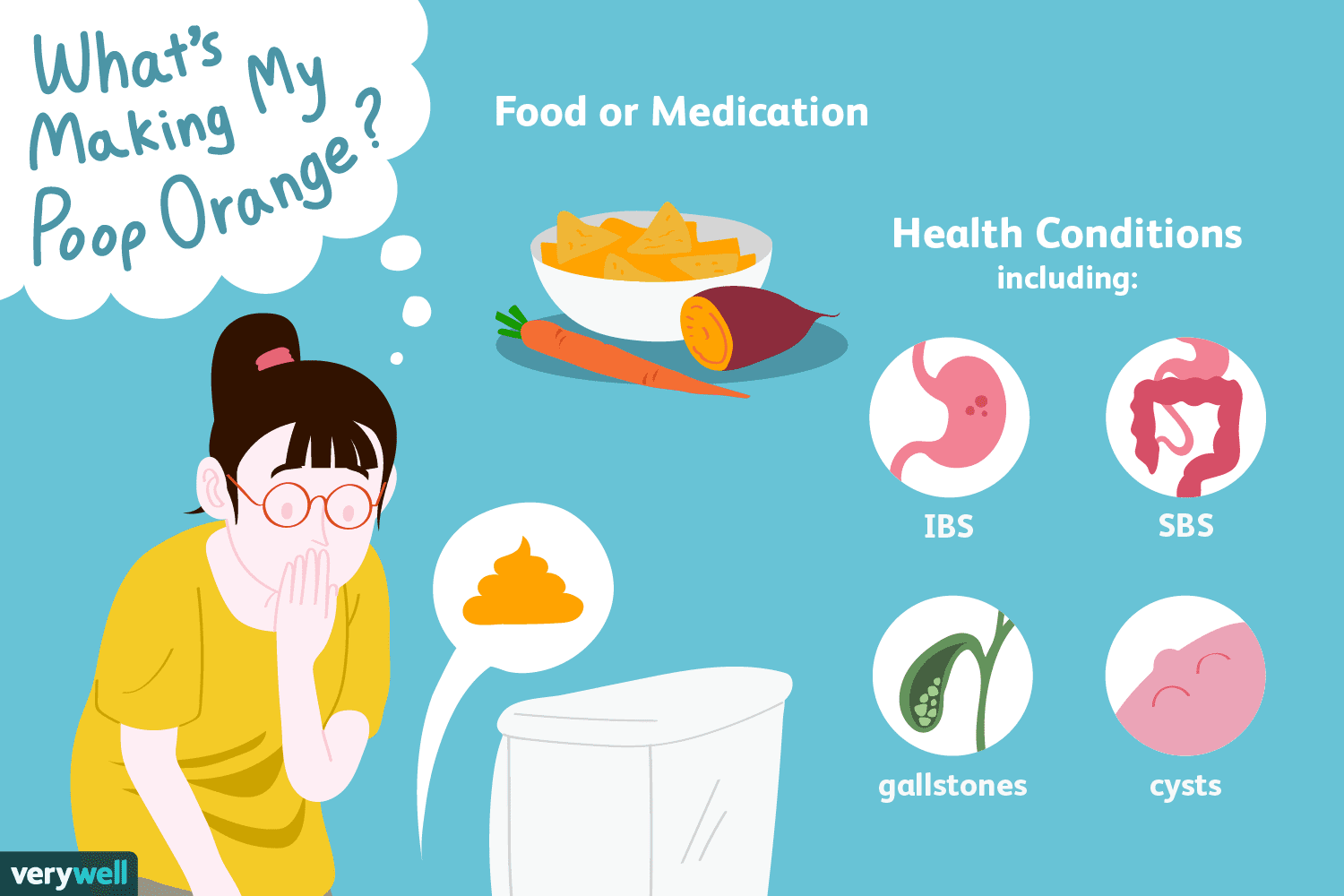 Firwat Dir vläicht orange Hocker hutt
Wann et orange Hocker ass, ass et héchstwahrscheinlech wéinst Iessen iessen déi orange a Faarf sinn (entweder natierlech oder kënschtlech Faarf, déi éischter vill méi laang daueren an hunn méi déif Fa
Firwat Dir vläicht orange Hocker hutt
Wann et orange Hocker ass, ass et héchstwahrscheinlech wéinst Iessen iessen déi orange a Faarf sinn (entweder natierlech oder kënschtlech Faarf, déi éischter vill méi laang daueren an hunn méi déif Fa
 Meng SIBO Atemtestresultater kréien
Déi lescht Woch hunn ech mat Iech gedeelt firwat ech fir SIBO nei getest hunn , dräi Joer no menger ursprénglecher Diagnos. Et war zimmlech komescht Gefill, duerch dPréparatioun Diät ze goen, wéi ech
Meng SIBO Atemtestresultater kréien
Déi lescht Woch hunn ech mat Iech gedeelt firwat ech fir SIBO nei getest hunn , dräi Joer no menger ursprénglecher Diagnos. Et war zimmlech komescht Gefill, duerch dPréparatioun Diät ze goen, wéi ech
 Wat sinn d'Unzeeche vu Bauchproblemer?
Firwat mécht mäi Mo wéi? Léiert iwwer Unzeeche vu Bauchproblemer a wat se verursaache kënnen Bauchprobleemer sinn typesch mam Verdauungstrakt an dResultat vu verschiddene Konditiounen, déi dVerdauung
Wat sinn d'Unzeeche vu Bauchproblemer?
Firwat mécht mäi Mo wéi? Léiert iwwer Unzeeche vu Bauchproblemer a wat se verursaache kënnen Bauchprobleemer sinn typesch mam Verdauungstrakt an dResultat vu verschiddene Konditiounen, déi dVerdauung