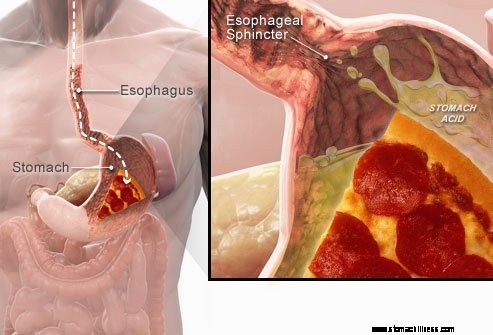
 Ko pogoltnete hrano, potuje po požiralniku navzdol in preide skozi mišični obroč, znan kot spodnji požiralni sfinkter ( LES). Ta struktura se odpre, da omogoči prehajanje hrane v želodec. Ostala naj bi zaprta, da bi vsebina želodca ostala tam, kjer sodi.
Ko pogoltnete hrano, potuje po požiralniku navzdol in preide skozi mišični obroč, znan kot spodnji požiralni sfinkter ( LES). Ta struktura se odpre, da omogoči prehajanje hrane v želodec. Ostala naj bi zaprta, da bi vsebina želodca ostala tam, kjer sodi.
Simptomi GERB ali refluksa kisline so posledica regurgitacije kisle tekoče želodčne vsebine nazaj v požiralnik. Najpogostejši simptom GERB je zgaga.
Drugi simptomi, ki se lahko pojavijo kot posledica GERB, vključujejo:
 Najpogostejši simptom GERB je zgaga.
Najpogostejši simptom GERB je zgaga. Gastroezofagealna refluksna bolezen, ki jo običajno imenujemo GERD ali refluks kisline, je stanje, pri katerem tekoča vsebina želodca regurgira (nazaj ali refluksira) v požiralnik. Tekočina lahko vname in poškoduje sluznico (ezofagitis), čeprav se vidni znaki vnetja pojavijo pri manjšini bolnikov. Regurgitirana tekočina običajno vsebuje kislino in pepsin, ki ju proizvaja želodec. (Pepsin je encim, ki začne prebavo beljakovin v želodcu.) Refluksirana tekočina lahko vsebuje tudi žolč, ki se je vrnil v želodec iz dvanajstnika. Prvi del tankega črevesa je pritrjen na želodec. Verjame se, da je kislina najbolj škodljiva sestavina refluksirane tekočine. Pepsin in žolč lahko tudi poškodujeta požiralnik, vendar njihova vloga pri nastajanju vnetja in poškodb požiralnika ni tako jasna kot vloga kisline.
GERB je kronična bolezen. Ko se enkrat začne, je običajno vseživljenjsko. Če pride do poškodbe sluznice požiralnika (ezofagitis), je to tudi kronično stanje. Poleg tega se po zacelitvi požiralnika z zdravljenjem in prekinitvi zdravljenja poškodba pri večini bolnikov vrne v nekaj mesecih. Ko se zdravljenje GERB začne, ga bo treba nadaljevati za nedoločen čas. Vendar pa je nekatere bolnike z občasnimi simptomi in brez ezofagitisa mogoče zdraviti le v simptomatskih obdobjih.
Pravzaprav se pri večini normalnih posameznikov pojavi refluks želodčne tekoče vsebine v požiralnik. Ena študija je pokazala, da se refluks pogosto pojavlja pri normalnih posameznikih, kot pri bolnikih z GERB. Pri bolnikih z GERB pa refluksirana tekočina pogosteje vsebuje kislino, kislina pa ostane v požiralniku dlje. Ugotovljeno je bilo tudi, da se pri bolnikih z GERB refluks tekočine v požiralniku višji kot pri normalnih posameznikih.
Kot se pogosto zgodi, ima telo načine, da se zaščiti pred škodljivimi učinki refluksa in kisline. Na primer, večina refluksa se pojavi čez dan, ko so posamezniki pokonci. V pokončnem položaju je večja verjetnost, da bo refluksirana tekočina zaradi učinka gravitacije stekla nazaj v želodec. Poleg tega posamezniki, ko so budni, večkrat pogoltnejo, ne glede na to, ali gre za refluks ali ne. Vsak pogolt prenese vso refluksirano tekočino nazaj v želodec. Končno, žleze slinavke v ustih proizvajajo slino, ki vsebuje bikarbonat. Z vsakim zaužitkom potuje po požiralniku slina, ki vsebuje bikarbonat. Bikarbonat nevtralizira majhno količino kisline, ki ostane v požiralniku, potem ko gravitacija in požiranje odstrani večino kisle tekočine.
Gravitacija, požiranje in slina so pomembni zaščitni mehanizmi za požiralnik, vendar so učinkoviti le, če so posamezniki v pokončnem položaju. Ponoči med spanjem gravitacija nima učinka, požiranje se ustavi, zmanjša se izločanje sline. Zato je pri refluksu, ki se pojavi ponoči, večja verjetnost, da bo kislina dlje ostala v požiralniku in povzročila večjo poškodbo požiralnika.
Zaradi določenih pogojev je oseba dovzetna za GERB. Na primer, GERB je lahko resen problem med nosečnostjo. Povišane ravni hormonov v nosečnosti verjetno povzročijo refluks z znižanjem tlaka v spodnjem ezofagealnem sfinkterju (glejte spodaj). Hkrati naraščajoči plod poveča pritisk v trebuhu. Pričakovati je, da bosta oba učinka povečala refluks. Prav tako so bolniki z boleznimi, ki oslabijo mišice požiralnika, kot so skleroderma ali mešane bolezni vezivnega tkiva, bolj nagnjene k razvoju GERB.
Vzrok za GERB je zapleten in lahko vključuje več vzrokov. Poleg tega lahko različni vzroki vplivajo na različne posameznike ali celo na istega posameznika ob različnih časih. Majhno število bolnikov z GERB proizvaja nenormalno velike količine kisline, vendar je to redko in ne prispeva k dejavniku pri veliki večini bolnikov.
Dejavniki, ki prispevajo k GERB, so:
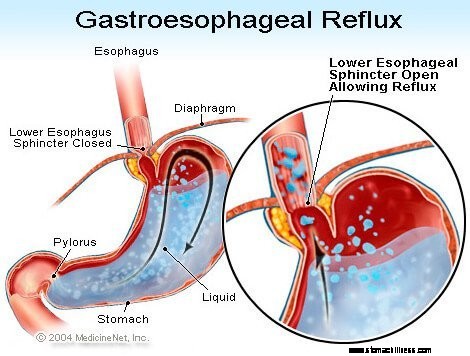
Delovanje spodnjega ezofagealnega sfinktra (LES) je morda najpomembnejši dejavnik (mehanizem) za preprečevanje refluksa. Požiralnik je mišična cev, ki sega od spodnjega grla do želodca. LES je specializiran mišični obroč, ki obdaja skrajni spodnji konec požiralnika, kjer se pridruži želodcu. Mišica, ki sestavlja LES, je večino časa aktivna, torej v mirovanju. To pomeni, da se krči in zapira prehod iz požiralnika v želodec. To zapiranje prehoda preprečuje refluks. Ko se hrana ali slina pogoltne, se LES za nekaj sekund sprosti, da hrana ali slina preide iz požiralnika v želodec, nato pa se spet zapre.
Pri bolnikih z GERB so odkrili več različnih nepravilnosti LES. Dva od njih vključujeta funkcijo LES. Prvi je nenormalno šibko krčenje LES, kar zmanjša njegovo sposobnost preprečevanja refluksa. Drugi so nenormalne sprostitve LES, imenovane prehodne relaksacije LES. Nenormalni so v tem, da ne spremljajo požiranja in trajajo dolgo, do nekaj minut. Te dolgotrajne sprostitve omogočajo lažje pojavljanje refluksa. Prehodne relaksacije LES se pri bolnikih z GERB najpogosteje pojavijo po obrokih, ko je želodec raztegnjen s hrano. Prehodne sprostitve LES se pojavljajo tudi pri posameznikih brez GERB, vendar so redke.
Najnovejša opisana nenormalnost pri bolnikih z GERB je ohlapnost LES. Natančneje, podobni napihnjeni pritiski bolj odpirajo LES pri bolnikih z GERB kot pri posameznikih brez GERB. Vsaj teoretično bi to omogočilo lažje odpiranje LES in/ali večji povratni tok kisline v požiralnik, ko je LES odprt.
Hiatalne kile prispevajo k refluksu, čeprav način, na katerega prispevajo, ni jasen. Večina bolnikov z GERB ima hiatalno kilo, mnogi pa ne. Zato za GERB ni nujno imeti hiatalne kile. Poleg tega ima veliko ljudi hiatalne kile, vendar nimajo GERB. Ni natančno znano, kako in zakaj se razvijejo hiatalne kile.
Običajno se LES nahaja na isti ravni, kjer požiralnik prehaja iz prsnega koša skozi majhno odprtino v diafragmi in v trebuh. (Diafragma je mišičasta, vodoravna pregrada, ki ločuje prsni koš od trebuha.) Ko je hiatalna kila, majhen del zgornjega želodca, ki se pritrdi na požiralnik, potisne navzgor skozi diafragmo. Posledično majhen del želodca in LES ležita v prsnem košu, LES pa ni več na ravni diafragme.
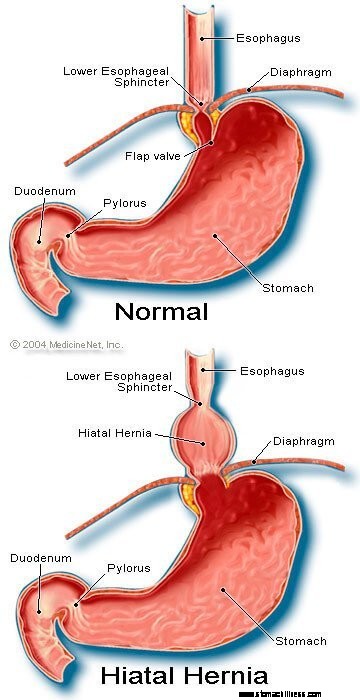 Slika hiatalne kile
Slika hiatalne kile
Zdi se, da je diafragma, ki obdaja LES, pomembna pri preprečevanju refluksa. To pomeni, da je pri posameznikih brez hiatalne kile diafragma, ki obdaja požiralnik, neprekinjeno krčena, nato pa se s požiranjem sprosti, tako kot LES. Upoštevajte, da se učinki LES in diafragme pojavijo na istem mestu pri bolnikih brez hiatalne kile. Zato je ovira za refluks enaka vsoti tlakov, ki jih ustvarita LES in diafragma. Ko se LES premakne v prsni koš s hiatalno kilo, diafragma in LES še naprej izvajata pritisk in pregradni učinek. Vendar to zdaj počnejo na različnih lokacijah. Posledično tlaki niso več aditivni. Namesto tega eno samo visokotlačno oviro za refluks nadomestita dve oviri nižjega tlaka in refluks se tako lažje pojavi. Torej je zmanjšanje tlačne pregrade eden od načinov, kako lahko hiatalna kila prispeva k refluksu.
Kot smo že omenili, so lastovke pomembne pri odstranjevanju kisline v požiralniku. Požiranje povzroči obročast val krčenja mišic požiralnika, ki zoži lumen (notranjo votlino) požiralnika. Krčenje, imenovano peristaltika, se začne v zgornjem požiralniku in potuje v spodnji požiralnik. Potisne hrano, slino in vse, kar je v požiralniku, v želodec.
Ko je val krčenja okvarjen, se refluksirana kislina ne potisne nazaj v želodec. Pri bolnikih z GERB je bilo opisanih več nenormalnosti krčenja. Na primer, valovi krčenja se morda ne začnejo po vsakem zaužitju ali pa lahko valovi krčenja ugasnejo, preden dosežejo želodec. Tudi pritisk, ki ga povzročajo kontrakcije, je lahko prešibek, da bi potisnil kislino nazaj v želodec. Takšne nenormalnosti krčenja, ki zmanjšajo očistek kisline iz požiralnika, pogosto najdemo pri bolnikih z GERB. Pravzaprav jih najpogosteje najdemo pri tistih bolnikih z najhujšo GERB. Pričakovati je, da bodo učinki nenormalnih kontrakcij požiralnika hujši ponoči, ko gravitacija ne pomaga vračati refluksirane kisline v želodec. Upoštevajte, da kajenje tudi znatno zmanjša očistek kisline iz požiralnika. Ta učinek traja vsaj 6 ur po zadnji cigareti.
Večina refluksa čez dan se pojavi po obroku. Ta refluks je verjetno posledica prehodnih sprostitev LES, ki jih povzroči napenjanje želodca s hrano. Pri manjšini bolnikov z GERB je bilo ugotovljeno, da ima želodce, ki se po obroku nenormalno počasi praznijo. To se imenuje gastropareza. Počasnejše praznjenje želodca podaljša napenjanje želodca s hrano po obroku. Zato počasnejše praznjenje podaljša čas, v katerem je verjetneje, da se pojavi refluks. Obstaja več zdravil, povezanih z motenim praznjenjem želodca, kot so:
Posamezniki ne smejo prenehati jemati teh ali kakršnih koli predpisanih zdravil, dokler se zdravnik, ki jih predpisuje, ne pogovori z njimi o morebitni situaciji GERB.
Simptomi nezapletene GERB so predvsem:
Drugi simptomi se pojavijo, ko pride do zapletov GERB, in o njih bomo razpravljali.
Ko se kislina refluksira nazaj v požiralnik pri bolnikih z GERB, se živčna vlakna v požiralniku stimulirajo. Ta živčna stimulacija najpogosteje povzroči zgago, bolečino, ki je značilna za GERB. Zgaga je običajno opisana kot pekoča bolečina v sredini prsnega koša. Lahko se začne visoko v trebuhu ali pa sega do vratu. Pri nekaterih bolnikih pa je bolečina lahko ostra ali podobna pritisku, ne pa pekoča. Takšna bolečina lahko posnema bolečino v srcu (angino pektoris). Pri drugih bolnikih se bolečina lahko razširi v hrbet.
Ker je refluks kisline pogostejši po obroku, je zgaga pogostejša po obroku. Zgaga je pogostejša tudi, ko posamezniki leže, saj brez učinkov gravitacije refluks poteka lažje, kislina pa se počasneje vrača v želodec. Številne bolnike z GERB iz spanja zbudi zgaga.
Epizode zgage se običajno pojavijo občasno. To pomeni, da so epizode pogostejše ali hujše v obdobju več tednov ali mesecev, nato pa postanejo manj pogoste ali hude ali celo odsotne več tednov ali mesecev. Ta periodičnost simptomov je razlog za občasno zdravljenje pri bolnikih z GERB, ki nimajo ezofagitisa. Kljub temu je zgaga življenjska težava in se skoraj vedno vrne.
Regurgitacija je pojav refluksne tekočine v ustih. Pri večini bolnikov z GERB običajno le majhne količine tekočine dosežejo požiralnik, tekočina pa ostane v spodnjem požiralniku. Občasno se pri nekaterih bolnikih z GERB večje količine tekočine, ki včasih vsebuje hrano, refluksirajo in dosežejo zgornji požiralnik.
Na zgornjem koncu požiralnika je zgornji ezofagealni sfinkter (UES). UES je krožni mišični obroč, ki je po svojih dejanjih zelo podoben LES. To pomeni, da UES preprečuje, da bi se vsebina požiralnika vrnila nazaj v grlo. Ko majhne količine refluksirane tekočine in/ali hrane pridejo mimo UES in pridejo v grlo, se lahko v ustih pojavi kisel okus. Če večje količine prodrejo v UES, lahko bolniki nenadoma ugotovijo, da so njihova usta napolnjena s tekočino ali hrano. Še več, pogosta ali dolgotrajna regurgitacija lahko povzroči erozije zob, ki jih povzroča kislina.
Slabost je pri GERB redka. Pri nekaterih bolnikih pa je lahko pogosta ali huda in lahko povzroči bruhanje. Pravzaprav je pri bolnikih z nepojasnjeno slabostjo in/ali bruhanjem GERB eden prvih pogojev, ki jih je treba upoštevati. Ni jasno, zakaj nekateri bolniki z GERB razvijejo predvsem zgago, drugi pa predvsem slabost.
Tekočina iz želodca, ki refluksira v požiralnik, poškoduje celice, ki obdajajo požiralnik. Telo se odzove tako, kot se običajno odzove na poškodbe, to je z vnetjem (ezofagitis). Namen vnetja je nevtralizirati škodljivo sredstvo in začeti proces celjenja. Če poškodba gre globoko v požiralnik, nastane razjeda. Razjeda je preprosto zlom sluznice požiralnika, ki se pojavi na območju vnetja. Razjede in dodatna vnetja, ki jih povzročajo, lahko erodirajo v krvne žile požiralnika in povzročijo krvavitev v požiralnik.
Občasno je krvavitev huda in lahko zahteva:
Razjede na požiralniku se zacelijo s tvorbo brazgotin (fibroze). Sčasoma se brazgotinsko tkivo skrči in zoži lumen (notranjo votlino) požiralnika. To brazgotinsko zoženje imenujemo striktura. Zaužita hrana se lahko zatakne v požiralniku, ko postane zožitev dovolj močna (običajno, ko omeji lumen požiralnika na premer enega centimetra). Ta situacija lahko zahteva endoskopsko odstranitev zataknjene hrane. Nato, da se hrana ne bi prijela, je treba zožitev raztegniti (razširiti). Poleg tega je treba preprečiti tudi refluks, da preprečimo ponovitev strikture.
Dolgotrajna in/ali huda GERB pri nekaterih bolnikih povzroči spremembe v celicah, ki obdajajo požiralnik. Te celice so predrakave in lahko, čeprav običajno, postanejo rakave. To stanje se imenuje Barrettov požiralnik in se pojavi pri približno 10 % bolnikov z GERB. Vrsta raka požiralnika, povezana z Barrettovim požiralnikom (adenokarcinom), se pogosteje povečuje. Ni jasno, zakaj nekateri bolniki z GERB razvijejo Barrettov požiralnik, večina pa ne.
Barrettov požiralnik je mogoče vizualno prepoznati v času endoskopije in potrditi z mikroskopskim pregledom celic sluznice. Nato lahko bolnike z Barrettovim požiralnikom opravijo periodične nadzorne endoskopije z biopsijami, čeprav ni soglasja o tem, kateri bolniki potrebujejo nadzor. Namen nadzora je odkriti napredovanje od predrakavih sprememb v bolj rakave spremembe, da se lahko začne zdravljenje za preprečevanje raka. Verjame se tudi, da bi morali bolniki z Barrettovim požiralnikom prejemati maksimalno zdravljenje za GERB, da bi preprečili nadaljnjo poškodbo požiralnika. Preučujejo se postopki, ki odstranijo nenormalne celice obloge. Za odstranitev celic je mogoče uporabiti več endoskopskih, nekirurških tehnik. Te tehnike so privlačne, ker ne zahtevajo operacije; vendar so povezani z zapleti, dolgoročna učinkovitost zdravljenja pa še ni ugotovljena. Kirurška odstranitev požiralnika je vedno možnost.
V spodnjem delu požiralnika je veliko živcev. Nekatere od teh živcev stimulira refluksirana kislina in ta stimulacija povzroči bolečino (običajno zgaga). Drugi živci, ki so stimulirani, ne povzročajo bolečine. Namesto tega stimulirajo še druge živce, ki izzovejo kašelj. Na ta način lahko refluksirana tekočina povzroči kašelj, ne da bi sploh prišla do grla! Na podoben način lahko refluks v spodnji požiralnik stimulira živce požiralnika, ki se povezujejo in lahko stimulirajo živce, ki gredo v pljuča. Ti živci do pljuč lahko nato povzročijo zoženje manjših dihalnih cevi, kar povzroči napad astme.
Čeprav lahko GERB povzroči kašelj, ni pogost vzrok za nepojasnjen kašelj. Čeprav je lahko tudi GERB vzrok za astmo, je bolj verjetno, da povzroči astmatične napade pri bolnikih, ki že imajo astmo. Čeprav sta kronični kašelj in astma pogosti bolezni, ni jasno, kako pogosto ju poslabša ali povzroči GERB.
Če refluksirana tekočina pride mimo zgornjega ezofagealnega sfinktra, lahko vstopi v grlo (žrelo) in celo v glasovno škatlo (grlo). Nastalo vnetje lahko povzroči vneto grlo in hripavost. Tako kot pri kašljanju in astmi ni jasno, kako pogosto je GERB odgovorna za sicer nepojasnjeno vnetje žrela in grla.
Refluksirana tekočina, ki prehaja iz žrela (žrela) in v grlo, lahko pride v pljuča (aspiracija). Refluks tekočine v pljuča (imenovano aspiracija) pogosto povzroči kašelj in zadušitev. Aspiracija pa se lahko pojavi tudi brez teh simptomov. S temi simptomi ali brez njih lahko aspiracija povzroči okužbo pljuč in povzroči pljučnico. Ta vrsta pljučnice je resen problem, ki zahteva takojšnje zdravljenje. Kadar aspiracijo ne spremljajo simptomi, lahko povzroči počasno, progresivno brazgotinjenje pljuč (pljučna fibroza), ki ga lahko vidimo na rentgenskih slikah prsnega koša. Aspiracija se pogosteje pojavlja ponoči, ker takrat procesi (mehanizmi), ki ščitijo pred refluksom, niso aktivni in tudi refleks kašlja, ki ščiti pljuča, ni aktiven.
Grlo komunicira z nosnimi prehodi. Pri majhnih otrocih sta dve zaplati limfnega tkiva, imenovani adenoidi, locirani tam, kjer se zgornji del grla pridruži nosnim prehodom. Prehodi iz sinusov in cevi iz srednjih ušes (evstahijeve cevi) se odpirajo v zadnji del nosnih prehodov blizu adenoidov. Refluksirana tekočina, ki pride v zgornje grlo, lahko vname adenoide in povzroči njihovo otekanje. Otekli adenoidi lahko nato blokirajo prehode iz sinusov in Evstahijeve cevi. Ko se sinusi in srednja ušesa zaprejo iz nosnih poti zaradi otekanja adenoidov, se v njih nabira tekočina. To kopičenje tekočine lahko povzroči nelagodje v sinusih in ušesih. Ker so adenoidi izraziti pri majhnih otrocih in ne pri odraslih, je to kopičenje tekočine v ušesih in sinusih opaziti pri otrocih in ne pri odraslih.
Za diagnosticiranje in oceno bolnikov z GERB obstajajo številni postopki, testi in vrednotenje simptomov (na primer zgaga).
Običajen način za GERB je značilen simptom, zgaga. Zgaga je najpogosteje opisana kot sub-sternalno (pod sredino prsnega koša) pekoč občutek, ki se pojavi po obroku in se pogosto poslabša med ležanjem. Za potrditev diagnoze zdravniki pogosto zdravijo bolnike z zdravili, ki zavirajo nastajanje kisline v želodcu. Če se zgaga nato v veliki meri zmanjša, se šteje, da je diagnoza GERB potrjena. Ta pristop postavljanja diagnoze na podlagi odziva simptomov na zdravljenje se običajno imenuje terapevtsko preskušanje.
S tem pristopom obstajajo težave. Na primer, bolniki, ki imajo stanja, ki lahko posnemajo GERB, zlasti razjedo na dvanajstniku ali želodcu (želodcu), se lahko tudi dejansko odzovejo na takšno zdravljenje. V tem primeru, če zdravnik domneva, da je težava GERB, bi bil vzrok za ulkusno bolezen spregledan, kot je vrsta okužbe, imenovana Helicobacter pylori (H. pylori ), ali nesteroidna protivnetna zdravila ali nesteroidna protivnetna zdravila (na primer ibuprofen), lahko povzročijo tudi razjede in ta stanja bi se obravnavala drugače kot GERB.
Poleg tega, tako kot pri vsakem zdravljenju, obstaja morda 20 % placebo učinek, kar pomeni, da se bo 20 % bolnikov odzvalo na placebo (neaktivno) tableto ali dejansko na katero koli zdravljenje. To pomeni, da se bo pri 20 % bolnikov, ki imajo vzroke za simptome, ki niso GERB (ali razjede), simptomi po zdravljenju GERB zmanjšali. Tako se bodo ti bolniki na podlagi njihovega odziva na zdravljenje (terapevtsko preskušanje) še naprej zdravili zaradi GERB, čeprav nimajo GERB. Še več, resničnega vzroka njihovih simptomov ne bomo iskali.
Endoskopija zgornjega prebavil (znana tudi kot esophago-gastro-duodenoscopy ali EGD) je pogost način diagnosticiranja GERB. EGD je postopek, pri katerem se pogoltne cev, ki vsebuje optični sistem za vizualizacijo. Ko cev napreduje navzdol po prebavilih, lahko pregledamo sluznico požiralnika, želodca in dvanajstnika.
Požiralnik večine bolnikov s simptomi refluksa je videti normalen. Zato pri večini bolnikov endoskopija ne bo pomagala pri diagnozi GERB. Vendar se včasih zdi, da je sluznica požiralnika vneta (ezofagitis). Poleg tega, če opazimo erozije (površinske zlome sluznice požiralnika) ali razjede (globlje zlome sluznice), je mogoče zanesljivo postaviti diagnozo GERB. Endoskopija bo odkrila tudi več zapletov GERB, zlasti razjede, strikture in Barrettov požiralnik. Lahko se dobijo tudi biopsije.
Nazadnje je mogoče z EGD diagnosticirati druge pogoste težave, ki lahko povzročajo simptome, podobne GERB (na primer razjede, vnetje ali rak na želodcu ali dvanajstniku).
Biopsije požiralnika, pridobljene z endoskopom, se ne štejejo za zelo koristne za diagnosticiranje GERB. Vendar pa so uporabni pri diagnosticiranju raka ali vzrokov vnetja požiralnika, razen refluksa kisline, zlasti okužb. Poleg tega so biopsije edini način za diagnosticiranje celičnih sprememb Barrettovega požiralnika. V zadnjem času je bilo predlagano, da tudi pri bolnikih z GERB, katerih požiralniki se očesu zdijo normalni, bodo biopsije pokazale razširitev prostora med celicami obloge, kar je morda znak poškodbe. Vendar je še prezgodaj sklepati, da je opazovanje širitve dovolj specifično, da bi lahko bili prepričani, da je GERB prisoten.
Pred uvedbo endoskopije je bila rentgenska slika požiralnika (imenovana ezofagram) edino sredstvo za diagnosticiranje GERB. Bolniki so pogoltnili barij (kontrastni material), nato pa so bili rentgenski posnetki požiralnika, napolnjenega z barijem. Težava s požiralnikom je bila, da je bil neobčutljiv test za diagnosticiranje GERB. To pomeni, da pri mnogih bolnikih, ki so imeli GERB, ni bilo mogoče najti znakov GERB, ker so imeli le malo ali nič poškodb sluznice požiralnika. Rentgenski žarki so lahko pokazali le redke zaplete GERB, na primer razjede in strikture. Rentgenski žarki so bili opuščeni kot sredstvo za diagnosticiranje GERB, čeprav so še vedno lahko uporabni skupaj z endoskopijo pri ocenjevanju zapletov.
Kadar GERB prizadene grlo ali grlo in povzroči simptome kašlja, hripavosti ali vnetja grla, bolniki pogosto obiščejo specialista za ušesa, nos in grlo (ENT). ORL specialist pogosto odkrije znake vnetja žrela ali grla. Čeprav so bolezni grla ali grla običajno vzrok za vnetje, je včasih vzrok lahko tudi GERB. V skladu s tem strokovnjaki ORL pogosto poskušajo zdravljenje z zaviranjem kisline, da potrdijo diagnozo GERB. Vendar ima ta pristop enake težave, kot so opisane zgoraj, ki so posledica uporabe odziva na zdravljenje za potrditev GERB.
Testiranje ezofagealne kisline velja za "zlati standard" za diagnosticiranje GERB. Kot smo že omenili, je refluks kisline pogost v splošni populaciji. Vendar pa imajo bolniki s simptomi ali zapleti GERB refluks več kisline kot posamezniki brez simptomov ali zapletov GERB. Poleg tega se lahko normalni posamezniki in bolniki z GERB med seboj zmerno dobro ločijo po dolžini časa, v katerem požiralnik vsebuje kislino.
Čas, v katerem požiralnik vsebuje kislino, se določi s testom, imenovanim 24-urni pH test požiralnika. (pH je matematični način za izražanje količine kislosti.) Za ta test se majhna cev (kateter) spelje skozi nos in namesti v požiralnik. Na konici katetra je senzor, ki zaznava kislino. Drugi konec katetra izstopi iz nosu, se ovije nazaj čez uho in potuje navzdol do pasu, kjer je pritrjen na snemalnik. Vsakič, ko se kislina iz želodca vrne nazaj v požiralnik, stimulira senzor in snemalnik zabeleži epizodo refluksa. Po 20 do 24-urnem časovnem obdobju se kateter odstrani in analizira zapis refluksa iz snemalnika.
Obstajajo težave z uporabo pH testiranja za diagnosticiranje GERB. Kljub dejstvu, da je normalne posameznike in bolnike z GERB mogoče dokaj dobro ločiti na podlagi pH študij, ločitev ni popolna. Zato bodo imeli nekateri bolniki z GERB normalne količine refluksa kisline, nekateri bolniki brez GERB pa nenormalne količine refluksa kisline. Za potrditev prisotnosti GERB je potrebno nekaj drugega kot test pH, na primer tipični simptomi, odziv na zdravljenje ali prisotnost zapletov GERB. GERB se lahko zanesljivo diagnosticira tudi, če epizode zgage korelirajo z refluksom kisline, kot je razvidno s testiranjem kisline.
Testiranje pH se uporablja pri obvladovanju GERB, razen le pri diagnosticiranju GERB. Na primer, test lahko pomaga ugotoviti, zakaj se simptomi GERB ne odzivajo na zdravljenje. Morda se pri 10 do 20 odstotkih bolnikov simptomi z zdravljenjem GERB ne bodo bistveno izboljšali. To pomanjkanje odziva na zdravljenje je lahko posledica neučinkovitega zdravljenja. To pomeni, da zdravilo ne zavira ustrezno nastajanja kisline v želodcu in ne zmanjša refluksa kisline. Alternativno je pomanjkanje odziva mogoče razložiti z napačno diagnozo GERB. V obeh primerih je lahko pH test zelo koristen. Če testiranje med nadaljevanjem zdravljenja odkrije znaten refluks kisline, potem je zdravljenje neučinkovito in ga je treba spremeniti. Če testiranje pokaže dobro supresijo kisline z minimalnim refluksom kisline, je diagnoza GERB verjetno napačna in je treba poiskati druge vzroke za simptome.
Testiranje pH se lahko uporabi tudi za pomoč pri oceni, ali je refluks vzrok za simptome (običajno zgaga). Za izvedbo te ocene bolniki med izvajanjem 24-urnega ph testa zabeležijo vsakokrat, ko imajo simptome. Potem, ko se test analizira, se lahko ugotovi, ali se je v času simptomov pojavil refluks kisline ali ne. Če se je refluks pojavil hkrati s simptomi, je verjetno refluks vzrok za simptome. Če v času simptomov refluksa ni bilo, je malo verjetno, da bi bil refluks vzrok za simptome.
Nazadnje, pH testiranje se lahko uporabi za oceno bolnikov pred endoskopskim ali kirurškim zdravljenjem GERB. Kot je razloženo zgoraj, se bodo simptomi zmanjšali pri približno 20 % bolnikov, čeprav nimajo GERB (učinek placeba). Pred endoskopskim ali kirurškim zdravljenjem je pomembno, da te bolnike identificiramo, ker verjetno ne bodo imeli koristi od zdravljenja. Študija pH se lahko uporabi za identifikacijo teh bolnikov, ker bodo imeli normalne količine refluksa kisline.
A newer method for prolonged measurement (48 hours) of acid exposure in the esophagus utilizes a small, wireless capsule that is attached to the esophagus just above the LES. The capsule is passed to the lower esophagus by a tube inserted through either the mouth or the nose. After the capsule is attached to the esophagus, the tube is removed. The capsule measures the acid refluxing into the esophagus and transmits this information to a receiver that is worn at the waist. After the study, usually after 48 hours, the information from the receiver is downloaded into a computer and analyzed. The capsule falls off of the esophagus after 3-5 days and is passed in the stool. (The capsule is not reused.)
The advantage of the capsule over standard pH testing is that there is no discomfort from a catheter that passes through the throat and nose. Moreover, with the capsule, patients look normal (they don't have a catheter protruding from their noses) and are more likely to go about their daily activities, for example, go to work, without feeling self-conscious. Because the capsule records for a longer period than the catheter (48 versus 24 hours), more data on acid reflux and symptoms are obtained. Nevertheless, it is not clear whether obtaining additional information is important.
Capsule pH testing is expensive. Sometimes the capsule does not attach to the esophagus or falls off prematurely. For periods of time the receiver may not receive signals from the capsule, and some of the information about reflux of acid may be lost. Occasionally there is pain with swallowing after the capsule has been placed, and the capsule may need to be removed endoscopically. Use of the capsule is an exciting use of new technology although it has its own specific problems.
Esophageal motility testing determines how well the muscles of the esophagus are working. For motility testing, a thin tube (catheter) is passed through a nostril, down the back of the throat, and into the esophagus. On the part of the catheter that is inside the esophagus are sensors that sense pressure. A pressure is generated within the esophagus that is detected by the sensors on the catheter when the muscle of the esophagus contracts. The end of the catheter that protrudes from the nostril is attached to a recorder that records the pressure. During the test, the pressure at rest and the relaxation of the lower esophageal sphincter are evaluated. The patient then swallows sips of water to evaluate the contractions of the esophagus.
Esophageal motility testing has two important uses in evaluating GERD. The first is in evaluating symptoms that do not respond to treatment for GERD since the abnormal function of the esophageal muscle sometimes causes symptoms that resemble the symptoms of GERD. Motility testing can identify some of these abnormalities and lead to a diagnosis of an esophageal motility disorder. The second use is evaluation prior to surgical or endoscopic treatment for GERD. In this situation, the purpose is to identify patients who also have motility disorders of the esophageal muscle. The reason for this is that in patients with motility disorders, some surgeons will modify the type of surgery they perform for GERD.
Gastric emptying studies are studies that determine how well food empties from the stomach. As discussed above, about 20 % of patients with GERD have slow emptying of the stomach that may be contributing to the reflux of acid. For gastric emptying studies, the patient eats a meal that is labeled with a radioactive substance. A sensor that is similar to a Geiger counter is placed over the stomach to measure how quickly the radioactive substance in the meal empties from the stomach.
Information from the emptying study can be useful for managing patients with GERD. For example, if a patient with GERD continues to have symptoms despite treatment with the usual medications, doctors might prescribe other medications that speed-up emptying of the stomach. Alternatively, in conjunction with GERD surgery, they might do a surgical procedure that promotes a more rapid emptying of the stomach. Nevertheless, it is still debated whether a finding of reduced gastric emptying should prompt changes in the surgical treatment of GERD.
Symptoms of nausea, vomiting, and regurgitation may be due either to abnormal gastric emptying or GERD. An evaluation of gastric emptying, therefore, may be useful in identifying patients whose symptoms are due to abnormal emptying of the stomach rather than to GERD.
The acid perfusion (Bernstein) test is used to determine if chest pain is caused by acid reflux. For the acid perfusion test, a thin tube is passed through one nostril, down the back of the throat, and into the middle of the esophagus. A dilute, acid solution and a physiologic salt solution (similar to the fluid that bathes the body's cells) are alternately poured (perfused) through the catheter and into the esophagus. The patient is unaware of which solution is being infused. If the perfusion with acid provokes the patient's usual pain and perfusion of the salt solution produces no pain, it is likely that the patient's pain is caused by acid reflux.
The acid perfusion test, however, is used only rarely. A better test for correlating pain and acid reflux is a 24-hour esophageal pH or pH capsule study during which patients note when they are having pain. It then can be determined from the pH recording if there was an episode of acid reflux at the time of the pain. This is the preferable way of deciding if acid reflux is causing a patient's pain. It does not work well, however, for patients who have infrequent pain, for example every two to three days, which may be missed by a one or two day pH study. In these cases, an acid perfusion test may be reasonable.
One of the simplest treatments for GERD is referred to as life-style changes, a combination of several changes in habit, particularly related to eating.
As discussed above, reflux of acid is more injurious at night than during the day. At night, when individuals are lying down, it is easier for reflux to occur. The reason that it is easier is because gravity is not opposing the reflux, as it does in the upright position during the day. In addition, the lack of an effect of gravity allows the refluxed liquid to travel further up the esophagus and remain in the esophagus longer. These problems can be overcome partially by elevating the upper body in bed. The elevation is accomplished either by putting blocks under the bed's feet at the head of the bed or, more conveniently, by sleeping with the upper body on a foam rubber wedge. These maneuvers raise the esophagus above the stomach and partially restore the effects of gravity. It is important that the upper body and not just the head be elevated. Elevating only the head does not raise the esophagus and fails to restore the effects of gravity.
Elevation of the upper body at night generally is recommended for all patients with GERD. Nevertheless, most patients with GERD have reflux only during the day and elevation at night is of little benefit for them. It is not possible to know for certain which patients will benefit from elevation at night unless acid testing clearly demonstrates night reflux. However, patients who have heartburn, regurgitation, or other symptoms of GERD at night are probably experiencing reflux at night and definitely should elevate their upper body when sleeping. Reflux also occurs less frequently when patients lie on their left rather than their right sides.
Several changes in eating habits can be beneficial in treating GERD. Reflux is worse following meals. This probably is so because the stomach is distended with food at that time and transient relaxations of the lower esophageal sphincter are more frequent. Therefore, smaller and earlier evening meals may reduce the amount of reflux for two reasons. First, the smaller meal results in lesser distention of the stomach. Second, by bedtime, a smaller and earlier meal is more likely to have emptied from the stomach than is a larger one. As a result, reflux is less likely to occur when patients with GERD lie down to sleep.
Certain foods are known to reduce the pressure in the lower esophageal sphincter and thereby promote reflux. These foods should be avoided and include:
Fatty foods (which should be decreased) and smoking (which should be stopped) also reduce the pressure in the sphincter and promote reflux.
In addition, patients with GERD may find that other foods aggravate their symptoms. Examples are spicy or acid-containing foods, like citrus juices, carbonated beverages, and tomato juice. These foods should also be avoided if they provoke symptoms.
One novel approach to the treatment of GERD is chewing gum. Chewing gum stimulates the production of more bicarbonate-containing saliva and increases the rate of swallowing. After the saliva is swallowed, it neutralizes acid in the esophagus. In effect, chewing gum exaggerates one of the normal processes that neutralize acid in the esophagus. It is not clear, however, how effective chewing gum is in treating heartburn. Nevertheless, chewing gum after meals is certainly worth a try.
There is a variety of over-the-counter (for example, antacids and foam barriers) and prescription medications (for example, proton pump inhibitors, histamine antagonists, and promotility drugs) for treating GERD.
Despite the development of potent medications for the treatment of GERD, antacids remain a mainstay of treatment. Antacids neutralize the acid in the stomach so that there is no acid to reflux. The problem with antacids is that their action is brief. They are emptied from the empty stomach quickly, in less than an hour, and the acid then re-accumulates. The best way to take antacids, therefore, is approximately one hour after meals, which is just before the symptoms of reflux begin after a meal. Since the food from meals slows the emptying from the stomach, an antacid taken after a meal stays in the stomach longer and is effective longer. For the same reason, a second dose of antacids approximately two hours after a meal takes advantage of the continuing post-meal slower emptying of the stomach and replenishes the acid-neutralizing capacity within the stomach.
Antacids may be aluminum, magnesium, or calcium-based. Calcium-based antacids (usually calcium carbonate), unlike other antacids, stimulate the release of gastrin from the stomach and duodenum. Gastrin is the hormone that is primarily responsible for the stimulation of acid secretion by the stomach. Therefore, the secretion of acid rebounds after the direct acid-neutralizing effect of the calcium carbonate is exhausted. The rebound is due to the release of gastrin, which results in an overproduction of acid. Theoretically at least, this increased acid is not good for GERD.
Acid rebound, however, is not clinically important. That is, treatment with calcium carbonate is not less effective or safe than treatment with antacids not containing calcium carbonate. Nevertheless, the phenomenon of acid rebound is theoretically harmful. In practice, therefore, calcium-containing antacids such as Tums and Rolaids are not recommended for frequent use. The occasional use of these calcium carbonate-containing antacids, however, is not believed to be harmful. The advantages of calcium carbonate-containing antacids are their low cost, the calcium they add to the diet, and their convenience as compared to liquids.
Aluminum-containing antacids tend to cause constipation, while magnesium-containing antacids tend to cause diarrhea. If diarrhea or constipation becomes a problem, it may be necessary to switch antacids, or use antacids containing both aluminum and magnesium.
Although antacids can neutralize acid, they do so for only a short period. For substantial neutralization of acid throughout the day, antacids would need to be given frequently, at least every hour.
The first medication developed for the more effective and convenient treatment of acid-related diseases, including GERD, was a histamine antagonist, specifically cimetidine (Tagamet). Histamine is an important chemical because it stimulates acid production by the stomach. Released within the wall of the stomach, histamine attaches to receptors (binders) on the stomach's acid-producing cells and stimulates the cells to produce acid. Histamine antagonists work by blocking the receptor for histamine and thereby preventing histamine from stimulating the acid-producing cells. (Histamine antagonists are referred to as H2 antagonists because the specific receptor they block is the histamine type 2 receptor.)
As histamine is particularly important for the stimulation of acid after meals, H2 antagonists are best taken 30 minutes before meals. The reason for this timing is so that the H2 antagonists will be at peak levels in the body after the meal when the stomach is actively producing acid. H2 antagonists also can be taken at bedtime to suppress the nighttime production of acid.
H2 antagonists are very good for relieving the symptoms of GERD, particularly heartburn. However, they are not very good for healing the inflammation (esophagitis) that may accompany GERD. They are used primarily for the treatment of heartburn in GERD that is not associated with inflammation or complications, such as erosions or ulcers, strictures, or Barrett's esophagus.
Three different H2 antagonists are available by prescription, including cimetidine (Tagamet), nizatidine (Axid), and famotidine (Pepcid). Two of these, cimetidine (Tagamet HB) and famotidine (Pepcid AC, Zantac 360) are available over-the-counter (OTC), without the need for a prescription. However, the OTC dosages are lower than those available by prescription.
The second type of drug developed specifically for acid-related diseases, such as GERD, was a proton pump inhibitor (PPI), specifically, omeprazole (Prilosec). A PPI blocks the secretion of acid into the stomach by the acid-secreting cells. The advantage of a PPI over an H2 antagonist is that the PPI shuts off acid production more completely and for a longer period of time. Not only is the PPI good for treating the symptom of heartburn, but it also is good for protecting the esophagus from acid so that esophageal inflammation can heal.
PPIs are used when H2 antagonists do not relieve symptoms adequately or when complications of GERD such as erosions or ulcers, strictures, or Barrett's esophagus exist. Five different PPIs are approved for the treatment of GERD, including omeprazole (Prilosec, Dexilant), lansoprazole (Prevacid), rabeprazole (Aciphex), pantoprazole (Protonix), and esomeprazole (Nexium), and dexlansoprazole (Dexilant). A sixth PPI product consists of a combination of omeprazole and sodium bicarbonate (Zegerid). PPIs (except for Zegerid) are best taken an hour before meals. The reason for this timing is that the PPIs work best when the stomach is most actively producing acid, which occurs after meals. If the PPI is taken before the meal, it is at peak levels in the body after the meal when the acid is being made.
Pro-motility drugs work by stimulating the muscles of the gastrointestinal tract, including the esophagus, stomach, small intestine, and/or colon. One pro-motility drug, metoclopramide (Reglan), is approved for GERD. Pro-motility drugs increase the pressure in the lower esophageal sphincter and strengthen the contractions (peristalsis) of the esophagus. Both effects would be expected to reduce the reflux of acid. However, these effects on the sphincter and esophagus are small. Therefore, it is believed that the primary effect of metoclopramide may be to speed up emptying of the stomach, which also would be expected to reduce reflux.
Pro-motility drugs are most effective when taken 30 minutes before meals and again at bedtime. They are not very effective for treating either the symptoms or complications of GERD. Therefore, the pro-motility agents are reserved either for patients who do not respond to other treatments or are added to enhance other treatments for GERD.
Foam barriers provide a unique form of treatment for GERD. Foam barriers are tablets that are composed of an antacid and a foaming agent. As the tablet disintegrates and reaches the stomach, it turns into foam that floats on top of the liquid contents of the stomach. The foam forms a physical barrier to the reflux of liquid. At the same time, the antacid bound to the foam neutralizes acid that comes into contact with the foam. The tablets are best taken after meals (when the stomach is distended) and when lying down, both times when reflux is more likely to occur. Foam barriers are not often used as the first or only treatment for GERD. Rather, they are added to other drugs for GERD when the other drugs are not adequately effective in relieving symptoms. There is only one foam barrier, which is a combination of aluminum hydroxide gel, magnesium trisilicate, and alginate (Gaviscon).
The drugs described above usually are effective in treating the symptoms and complications of GERD. Nevertheless, sometimes they are not. For example, despite adequate suppression of acid and relief from heartburn, regurgitation, with its potential for complications in the lungs, may still occur. Moreover, the amounts and/or numbers of drugs that are required for satisfactory treatment are sometimes so great that drug treatment is unreasonable. In such situations, surgery can effectively stop reflux.
The surgical procedure that is done to prevent reflux is technically known as fundoplication and is called reflux surgery or anti-reflux surgery. During fundoplication, any hiatal hernial sac is pulled below the diaphragm and stitched there. In addition, the opening in the diaphragm through which the esophagus passes is tightened around the esophagus. Finally, the upper part of the stomach next to the opening of the esophagus into the stomach is wrapped around the lower esophagus to make an artificial lower esophageal sphincter. All of this surgery can be done through an incision in the abdomen (laparotomy) or using a technique called laparoscopy. During laparoscopy, a small viewing device and surgical instruments are passed through several small puncture sites in the abdomen. This procedure avoids the need for a major abdominal incision.
Surgery is very effective at relieving symptoms and treating the complications of GERD. Approximately 80% of patients will have good or excellent relief of their symptoms for at least 5 to 10 years. Nevertheless, many patients who have had surgery will continue to take drugs for reflux. It is not clear whether they take the drugs because they continue to have reflux and symptoms of reflux or if they take them for symptoms that are being caused by problems other than GERD. The most common complication of fundoplication is swallowed food that sticks at the artificial sphincter. Fortunately, the sticking usually is temporary. If it is not transient, endoscopic treatment to stretch (dilate) the artificial sphincter usually will relieve the problem. Only occasionally is it necessary to re-operate to revise the prior surgery.
Very recently, endoscopic techniques for the treatment of GERD have been developed and tested. One type of endoscopic treatment involves suturing (stitching) the area of the lower esophageal sphincter, which essentially tightens the sphincter.
A second type involves the application of radio-frequency waves to the lower part of the esophagus just above the sphincter. The waves cause damage to the tissue beneath the esophageal lining and a scar (fibrosis) forms. The scar shrinks and pulls on the surrounding tissue, thereby tightening the sphincter and the area above it.
A third type of endoscopic treatment involves the injection of materials into the esophageal wall in the area of the LES. The injected material is intended to increase pressure in the LES and thereby prevent reflux. In one treatment the injected material was a polymer. Unfortunately, the injection of polymer led to serious complications, and the material for injection is no longer available. Another treatment involving injection of expandable pellets also was discontinued. Limited information is available about a third type of injection which uses gelatinous polymethylmethacrylate microspheres.
Endoscopic treatment has the advantage of not requiring surgery. It can be performed without hospitalization. Experience with endoscopic techniques is limited. It is not clear how effective they are, especially long-term. Because the effectiveness and the full extent of potential complications of endoscopic techniques are not clear, it is felt generally that endoscopic treatment should only be done as part of experimental trials.
Transient LES relaxations appear to be the most common way in which acid reflux occurs. Although there is an available drug that prevents relaxations (baclofen), it has side effects that are too frequent to be generally useful. Much attention is being directed at the development of drugs that prevent these relaxations without accompanying side effects.
There are several ways to approach the evaluation and management of GERD. The approach depends primarily on the frequency and severity of symptoms, the adequacy of the response to treatment, and the presence of complications.
For infrequent heartburn, the most common symptom of GERD, life-style changes and an occasional antacid may be all that is necessary. If heartburn is frequent, daily non-prescription-strength (over-the-counter) H2 antagonists may be adequate. A foam barrier also can be used with the antacid or H2 antagonist.
If life-style changes and antacids, non-prescription H2 antagonists, and a foam barrier do not adequately relieve heartburn, it is time to see a physician for further evaluation and to consider prescription-strength drugs. The evaluation by the physician should include an assessment for possible complications of GERD based on the presence of such symptoms or findings as:
Clues to the presence of diseases that may mimic GERD, such as gastric or duodenal ulcers and esophageal motility disorders, should be sought.
If there are no symptoms or signs of complications and no suspicion of other diseases, a therapeutic trial of acid suppression with H2 antagonists often is used. If H2 antagonists are not adequately effective, a second trial, with the more potent PPIs, can be given. Sometimes, a trial of treatment begins with a PPI and skips the H2 antagonist. If treatment relieves the symptoms completely, no further evaluation may be necessary and the effective drug, the H2 antagonist or PPI, is continued. As discussed previously, however, there are potential problems with this commonly used approach, and some physicians would recommend a further evaluation for almost all patients they see.
If at the time of evaluation, there are symptoms or signs that suggest complicated GERD or a disease other than GERD or if the relief of symptoms with H2 antagonists or PPIs is not satisfactory, a further evaluation by endoscopy (EGD) definitely should be done.
There are several possible results of endoscopy and each requires a different approach to treatment. If the esophagus is normal and no other diseases are found, the goal of treatment simply is to relieve symptoms. Therefore, prescription strength H2 antagonists or PPIs are appropriate. If damage to the esophagus (esophagitis or ulceration) is found, the goal of treatment is healing the damage. In this case, PPIs are preferred over H2 antagonists because they are more effective for healing.
If complications of GERD, such as stricture or Barrett's esophagus are found, treatment with PPIs also is more appropriate. However, the adequacy of the PPI treatment probably should be evaluated with a 24-hour pH study during treatment with the PPI. (With PPIs, although the amount of acid reflux may be reduced enough to control symptoms, it may still be abnormally high. Therefore, judging the adequacy of suppression of acid reflux by only the response of symptoms to treatment is not satisfactory.) Strictures may also need to be treated by endoscopic dilatation (widening) of the esophageal narrowing. With Barrett's esophagus, periodic endoscopic examination should be done to identify pre-malignant changes in the esophagus.
If symptoms of GERD do not respond to maximum doses of PPI, there are two options for management. The first is to perform 24-hour pH testing to determine whether the PPI is ineffective or if a disease other than GERD is likely to be present. If the PPI is ineffective, a higher dose of PPI may be tried. The second option is to go ahead without 24 hour pH testing and to increase the dose of PPI. Another alternative is to add another drug to the PPI that works in a way that is different from the PPI, for example, a pro-motility drug or a foam barrier. If necessary, all three types of drugs can be used. If there is not a satisfactory response to this maximal treatment, 24 hour pH testing should be done.
Who should consider surgery or, perhaps, an endoscopic treatment trial for GERD? (As mentioned previously, the effectiveness of the recently developed endoscopic treatments remains to be determined.) Patients should consider surgery if they have regurgitation that cannot be controlled with drugs. This recommendation is particularly important if the regurgitation results in infections in the lungs or occurs at night when aspiration into the lungs is more likely. Patients also should consider surgery if they require large doses of PPI or multiple drugs to control their reflux. It is debated whether or not a desire to be free of the need to take life-long drugs to prevent symptoms of GERD is by itself a satisfactory reason for having surgery.
Some physicians - primarily surgeons - recommend that all patients with Barrett's esophagus should have surgery. This recommendation is based on the belief that surgery is more effective than endoscopic surveillance or ablation of the abnormal tissue followed by treatment with acid-suppressing drugs in preventing both the reflux and the cancerous changes in the esophagus. There are no studies, however, demonstrating the superiority of surgery over drugs or ablation for the treatment of GERD and its complications. Moreover, the effectiveness of drug treatment can be monitored with 24 hour pH testing.
One unresolved issue in GERD is the inconsistent relationships among acid reflux, heartburn, and damage to the lining of the esophagus (esophagitis and the complications).
Clearly, we have much to learn about the relationship between acid reflux and esophageal damage, and about the processes (mechanisms) responsible for heartburn. This issue is of more than passing interest. Knowledge of the mechanisms that produce heartburn and esophageal damage raises the possibility of new treatments that would target processes other than acid reflux.
One of the more interesting theories that has been proposed to answer some of these questions involves the reason for pain when acid refluxes. It often is assumed that the pain is caused by irritating acid contacting an inflamed esophageal lining. But the esophageal lining usually is not inflamed. It is possible therefore, that the acid is stimulating the pain nerves within the esophageal wall just beneath the lining. Although this may be the case, a second explanation is supported by the work of one group of scientists. These scientists find that heartburn provoked by acid in the esophagus is associated with contraction of the muscle in the lower esophagus. Perhaps it is the contraction of the muscle that somehow leads to the pain. It also is possible, however, that the contraction is an epiphenomenon, that is, refluxed acid stimulates pain nerves and causes the muscle to contract, but it is not the contraction that causes the pain. More studies will be necessary before the exact mechanism(s) that causes heartburn is clear.
There are potentially injurious agents that can be refluxed other than acid, for example, bile. Until recently it has been impossible or difficult to accurately identify non-acid reflux and, therefore, to study whether or not non-acid reflux is injurious or can cause symptoms.
A new technology allows the accurate determination of non-acid reflux. This technology uses the measurement of impedance changes within the esophagus to identify reflux of liquid, be it acid or non-acid. By combining measurement of impedance and pH it is possible to identify reflux and to tell if the reflux is acid or non-acid. It is too early to know how important non-acid reflux is in causing esophageal damage, symptoms, or complications, but there is little doubt that this new technology will be able to resolve the issues surrounding non-acid reflux.
 Ko dieta z nizko vsebnostjo FODMAP ne deluje pri IBS
Dieta z nizko vsebnostjo FODMAP je bila razvita kot način, da ljudem, ki imajo IBS, ponudimo prehranski pristop za obvladovanje motnje. Čeprav so osnovni vzroki za IBS zapleteni in niso popolnoma razu
Ko dieta z nizko vsebnostjo FODMAP ne deluje pri IBS
Dieta z nizko vsebnostjo FODMAP je bila razvita kot način, da ljudem, ki imajo IBS, ponudimo prehranski pristop za obvladovanje motnje. Čeprav so osnovni vzroki za IBS zapleteni in niso popolnoma razu
 »S spreminjanjem prehrane lahko spreminjate tudi svoje mikrobe«:intervju s Claro Belzer
Vse več znanstvenih študij kaže, da lahko prehrana vpliva na zdravje prek črevesne mikrobiote. »Z modulacijo vaše prehrane lahko modulirate tudi svoje mikrobe. Mikrobi lahko prispevajo k resnosti ali
»S spreminjanjem prehrane lahko spreminjate tudi svoje mikrobe«:intervju s Claro Belzer
Vse več znanstvenih študij kaže, da lahko prehrana vpliva na zdravje prek črevesne mikrobiote. »Z modulacijo vaše prehrane lahko modulirate tudi svoje mikrobe. Mikrobi lahko prispevajo k resnosti ali
 Refluks kisline:simptomi, dejavniki tveganja in zdravljenje
Če niste osebno izkusili refluksa kisline, ste verjetno že slišali zanj. Verjetno ste slišali tudi za zgago in GERB (gastroezofagealna refluksna bolezen). Čeprav te izraze mnogi ljudje uporabljajo izm
Refluks kisline:simptomi, dejavniki tveganja in zdravljenje
Če niste osebno izkusili refluksa kisline, ste verjetno že slišali zanj. Verjetno ste slišali tudi za zgago in GERB (gastroezofagealna refluksna bolezen). Čeprav te izraze mnogi ljudje uporabljajo izm