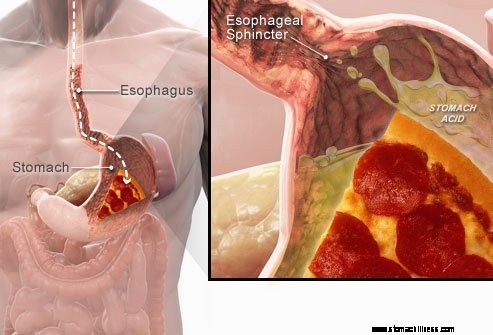
 Kada progutate hranu, ona putuje niz jednjak i prolazi kroz mišićni prsten poznat kao donji sfinkter jednjaka ( LES). Ova struktura se otvara kako bi hrana mogla proći u želudac. Trebao bi ostati zatvoren kako bi sadržaj želuca ostao tamo gdje mu je mjesto.
Kada progutate hranu, ona putuje niz jednjak i prolazi kroz mišićni prsten poznat kao donji sfinkter jednjaka ( LES). Ova struktura se otvara kako bi hrana mogla proći u želudac. Trebao bi ostati zatvoren kako bi sadržaj želuca ostao tamo gdje mu je mjesto.
Simptomi GERB-a ili refluksa kiseline uzrokovani su regurgitacijom kiselog tekućeg želučanog sadržaja natrag u jednjak. Najčešći simptom GERB-a je žgaravica.
Ostali simptomi koji se mogu pojaviti kao posljedica GERB-a uključuju:
 Najčešći simptom GERB-a je žgaravica.
Najčešći simptom GERB-a je žgaravica. Gastroezofagealna refluksna bolest, koja se obično naziva GERB ili refluks kiseline, stanje je u kojem tekući sadržaj želuca regurgira (nadoknađuje ili refluksira) u jednjak. Tekućina može upaliti i oštetiti sluznicu (ezofagitis), iako se vidljivi znakovi upale javljaju kod manjeg broja pacijenata. Regurgirana tekućina obično sadrži kiselinu i pepsin koje proizvodi želudac. (Pepsin je enzim koji započinje probavu proteina u želucu.) Refluksirana tekućina također može sadržavati žuč koja se vratila u želudac iz duodenuma. Prvi dio tankog crijeva pričvršćen za želudac. Vjeruje se da je kiselina najštetnija komponenta refluksirane tekućine. Pepsin i žuč također mogu ozlijediti jednjak, ali njihova uloga u stvaranju upale i oštećenja jednjaka nije tako jasna kao uloga kiseline.
GERB je kronično stanje. Jednom kada počne, obično traje doživotno. Ako postoji ozljeda sluznice jednjaka (ezofagitis), to je također kronično stanje. Štoviše, nakon što jednjak zacijeli liječenjem i prekine liječenje, ozljeda će se kod većine pacijenata vratiti u roku od nekoliko mjeseci. Jednom kada se započne liječenje GERB-a, morat će se nastaviti neograničeno. Međutim, neki pacijenti s povremenim simptomima i bez ezofagitisa mogu se liječiti samo tijekom simptomatskih razdoblja.
Zapravo, refluks želučane tekućine u jednjak javlja se kod većine normalnih osoba. Jedna studija je pokazala da se refluks često javlja u normalnih osoba kao i kod pacijenata s GERB-om. U bolesnika s GERB-om, međutim, refluksirana tekućina češće sadrži kiselinu, a kiselina se dulje zadržava u jednjaku. Također je utvrđeno da se tekućina refluksuje na višu razinu u jednjaku u bolesnika s GERB-om od normalnih osoba.
Kao što je često slučaj, tijelo ima načina da se zaštiti od štetnih učinaka refluksa i kiseline. Na primjer, većina refluksa događa se tijekom dana kada su pojedinci uspravni. U uspravnom položaju veća je vjerojatnost da će refluksirana tekućina teći natrag u želudac zbog učinka gravitacije. Osim toga, dok su pojedinci budni, oni stalno gutaju, bez obzira postoji li refluks ili ne. Svaki gutljaj nosi svu refluksiranu tekućinu natrag u želudac. Konačno, žlijezde slinovnice u ustima proizvode slinu koja sadrži bikarbonat. Svakim gutanjem pljuvačka koja sadrži bikarbonat putuje niz jednjak. Bikarbonat neutralizira malu količinu kiseline koja ostaje u jednjaku nakon što je gravitacija i gutanje uklonila većinu kisele tekućine.
Gravitacija, gutanje i slina važni su zaštitni mehanizmi za jednjak, ali su učinkoviti samo kada su pojedinci u uspravnom položaju. Noću tijekom spavanja gravitacija nema učinka, gutanje prestaje, a lučenje sline je smanjeno. Stoga je vjerojatnije da će refluks koji se javlja noću dovesti do duljeg zadržavanja kiseline u jednjaku i do većeg oštećenja jednjaka.
Određeni uvjeti čine osobu osjetljivom na GERB. Na primjer, GERB može biti ozbiljan problem tijekom trudnoće. Povišene razine hormona u trudnoći vjerojatno uzrokuju refluks snižavanjem tlaka u donjem sfinkteru jednjaka (vidi dolje). Istodobno, rastući fetus povećava pritisak u trbuhu. Očekuje se da će oba ova učinka povećati refluks. Također, bolesnici s bolestima koje slabe mišiće jednjaka, poput skleroderme ili mješovitih bolesti vezivnog tkiva, skloniji su razvoju GERB-a.
Uzrok GERB-a je složen i može uključivati više uzroka. Štoviše, različiti uzroci mogu utjecati na različite pojedince ili čak na istu osobu u različito vrijeme. Mali broj pacijenata s GERB-om proizvodi abnormalno velike količine kiseline, ali to je neuobičajeno i ne pridonosi čimbeniku u velikoj većini pacijenata.
Čimbenici koji doprinose GERB-u su:
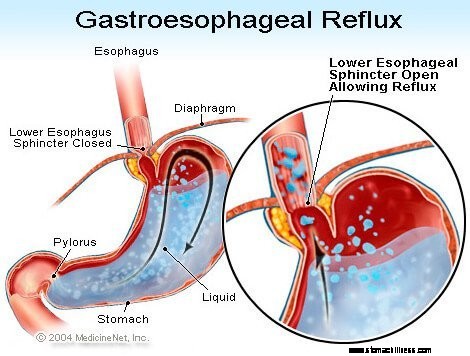
Djelovanje donjeg sfinktera jednjaka (LES) možda je najvažniji čimbenik (mehanizam) za sprječavanje refluksa. Jednjak je mišićna cijev koja se proteže od donjeg grla do želuca. LES je specijalizirani prsten mišića koji okružuje krajnji donji kraj jednjaka gdje se spaja sa želucem. Mišić koji čini LES aktivan je većinu vremena, odnosno u mirovanju. To znači da se skuplja i zatvara prolaz iz jednjaka u želudac. Ovo zatvaranje prolaza sprječava refluks. Kada se hrana ili slina proguta, LES se opušta na nekoliko sekundi kako bi omogućio da hrana ili slina prođu iz jednjaka u želudac, a zatim se ponovno zatvara.
U bolesnika s GERB-om pronađeno je nekoliko različitih abnormalnosti LES-a. Dvije od njih uključuju funkciju LES-a. Prvi je abnormalno slaba kontrakcija LES-a, što smanjuje njegovu sposobnost sprječavanja refluksa. Druga je abnormalna opuštanja LES-a, nazvana prolazna LES relaksacija. Nenormalni su po tome što ne prate lastavice i traju dugo, do nekoliko minuta. Ova dugotrajna opuštanja omogućuju lakše nastanak refluksa. Prolazne relaksacije LES-a javljaju se u bolesnika s GERB-om najčešće nakon jela kada je želudac nategnut hranom. Prolazne relaksacije LES također se javljaju u osoba bez GERB-a, ali su rijetke.
Posljednja opisana abnormalnost u bolesnika s GERB-om je labavost LES-a. Konkretno, slični rastezljivi pritisci otvaraju LES više u bolesnika s GERB-om nego u osoba bez GERB-a. Barem teoretski, to bi omogućilo lakše otvaranje LES-a i/ili veći povratni protok kiseline u jednjak kada je LES otvoren.
Hiatalne kile doprinose refluksu, iako nije jasan način na koji doprinose. Većina pacijenata s GERB-om ima hijatalnu kilu, ali mnogi nemaju. Stoga nije potrebno imati hijatalnu kilu da bi se dobio GERB. Štoviše, mnogi ljudi imaju hijatalne kile, ali nemaju GERB. Ne zna se sa sigurnošću kako i zašto nastaju hiatalne kile.
Normalno, LES se nalazi na istoj razini gdje jednjak prolazi iz prsnog koša kroz mali otvor na dijafragmi u trbuh. (Dijafragma je mišićava, horizontalna pregrada koja odvaja prsni koš od trbuha.) Kada postoji hijatalna kila, mali dio gornjeg dijela želuca koji se pričvršćuje za jednjak gura se prema gore kroz dijafragmu. Kao rezultat toga, mali dio želuca i LES leže u prsima, a LES više nije na razini dijafragme.
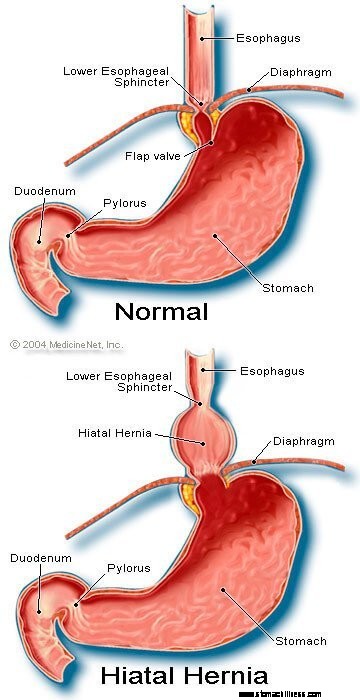 Slika hiatalne kile
Slika hiatalne kile
Čini se da je dijafragma koja okružuje LES važna u sprječavanju refluksa. Odnosno, u osoba bez hiatalne kile, dijafragma koja okružuje jednjak je kontinuirano kontrahirana, ali se zatim opušta gutanjem, baš kao i LES. Imajte na umu da se učinci LES-a i dijafragme javljaju na istom mjestu u bolesnika bez hiatalne kile. Stoga je barijera za refluks jednaka zbroju tlakova koje stvaraju LES i dijafragma. Kada se LES pomakne u prsni koš s hijatalnom hernijom, dijafragma i LES nastavljaju vršiti pritisak i učinak barijere. Međutim, sada to rade na različitim mjestima. Posljedično, pritisci više nisu aditivni. Umjesto toga, jedna visokotlačna barijera refluksu zamjenjuje se s dvije barijere nižeg tlaka, a refluks se tako događa lakše. Dakle, smanjenje barijere tlaka jedan je od načina na koji hiatalna hernija može doprinijeti refluksu.
Kao što je već spomenuto, lastavice su važne u eliminaciji kiseline u jednjaku. Gutanje uzrokuje prstenasti val kontrakcije mišića jednjaka, koji sužava lumen (unutarnju šupljinu) jednjaka. Kontrakcija, koja se naziva peristaltika, počinje u gornjem dijelu jednjaka i putuje do donjeg jednjaka. Gura hranu, slinu i sve ostalo u jednjaku u želudac.
Kada je val kontrakcije neispravan, refluksirana kiselina se ne gura natrag u želudac. U bolesnika s GERB-om opisano je nekoliko abnormalnosti kontrakcije. Na primjer, valovi kontrakcije možda neće početi nakon svakog gutanja ili valovi kontrakcije mogu izumrijeti prije nego što stignu u želudac. Također, pritisak koji stvaraju kontrakcije može biti preslab da bi gurnuo kiselinu natrag u želudac. Takve abnormalnosti kontrakcije, koje smanjuju klirens kiseline iz jednjaka, često se nalaze u bolesnika s GERB-om. Zapravo, najčešće se nalaze u onih bolesnika s najtežim GERB-om. Očekuje se da će učinci abnormalnih kontrakcija jednjaka biti gori noću kada gravitacija ne pomaže vraćanju refluksirane kiseline u želudac. Imajte na umu da pušenje također značajno smanjuje čišćenje kiseline iz jednjaka. Ovaj učinak traje najmanje 6 sati nakon posljednje cigarete.
Većina refluksa tijekom dana javlja se nakon jela. Ovaj refluks vjerojatno je posljedica prolaznih opuštanja LES-a koje su uzrokovane nadimanjem želuca hranom. Utvrđeno je da se kod manjeg broja pacijenata s GERB-om želuci nakon obroka nenormalno sporo prazni. To se zove gastropareza. Sporije pražnjenje želuca produljuje nadutost želuca hranom nakon jela. Stoga sporije pražnjenje produljuje vrijeme tijekom kojeg je vjerojatnije da će doći do refluksa. Postoji nekoliko lijekova povezanih s poremećenim pražnjenjem želuca, kao što su:
Pojedinci ne bi smjeli prestati uzimati ove ili bilo koje lijekove koji su propisani sve dok liječnik koji ih je propisao ne razgovara s njima o mogućoj situaciji s GERB-om.
Simptomi nekompliciranog GERB-a su prvenstveno:
Drugi simptomi se javljaju kada postoje komplikacije GERB-a i o njima će se raspravljati.
Kada se kiselina refluksira natrag u jednjak u bolesnika s GERB-om, stimuliraju se živčana vlakna u jednjaku. Ova stimulacija živaca najčešće rezultira žgaravicom, boli koja je karakteristična za GERB. Žgaravica se obično opisuje kao goruća bol u sredini prsnog koša. Može početi visoko u trbuhu ili se proširiti do vrata. U nekih pacijenata, međutim, bol može biti oštra ili nalik na pritisak, a ne žareća. Takva bol može oponašati bol u srcu (anginu). U drugih bolesnika bol se može proširiti na leđa.
Budući da je refluks kiseline češći nakon jela, žgaravica je češća nakon jela. Žgaravica je češća i kada pojedinci leže jer bez utjecaja gravitacije refluks se javlja lakše, a kiselina se sporije vraća u želudac. Mnoge pacijente s GERB-om iz sna probudi žgaravica.
Epizode žgaravice obično se događaju povremeno. To znači da su epizode češće ili teže u razdoblju od nekoliko tjedana ili mjeseci, a zatim postaju rjeđe ili teške ili čak izostaju nekoliko tjedana ili mjeseci. Ova periodičnost simptoma daje razlog za intermitentno liječenje bolesnika s GERB-om koji nemaju ezofagitis. Ipak, žgaravica je životni problem i gotovo uvijek se vraća.
Regurgitacija je pojava refluksirane tekućine u ustima. U većine bolesnika s GERB-om obično samo male količine tekućine dospiju u jednjak, a tekućina ostaje u donjem dijelu jednjaka. Povremeno se u nekih bolesnika s GERB-om refluksiraju veće količine tekućine, ponekad s hranom, i dospiju u gornji dio jednjaka.
Na gornjem kraju jednjaka nalazi se gornji ezofagealni sfinkter (UES). UES je kružni prsten mišića koji je po svom djelovanju vrlo sličan LES-u. To jest, UES sprječava povratak sadržaja jednjaka u grlo. Kada male količine refluksirane tekućine i/ili hrane prođu kroz UES i uđu u grlo, u ustima može postojati kiseli okus. Ako veće količine probiju UES, pacijenti mogu iznenada naći svoja usta puna tekućine ili hrane. Štoviše, česta ili dugotrajna regurgitacija može dovesti do kiselinskih erozija zuba.
Mučnina je rijetka pojava kod GERB-a. U nekih bolesnika, međutim, može biti česta ili teška i može rezultirati povraćanjem. Zapravo, u bolesnika s neobjašnjivom mučninom i/ili povraćanjem, GERB je jedno od prvih stanja koje treba uzeti u obzir. Nije jasno zašto neki pacijenti s GERB-om razvijaju uglavnom žgaravicu, a drugi uglavnom mučninu.
Tekućina iz želuca koja refluksira u jednjak oštećuje stanice koje oblažu jednjak. Tijelo reagira na način na koji obično reagira na oštećenja, a to je upalom (ezofagitis). Svrha upale je neutralizirati štetni agens i započeti proces ozdravljenja. Ako oštećenje ide duboko u jednjak, nastaje čir. Čir je jednostavno pukotina sluznice jednjaka koja se javlja u području upale. Čirevi i dodatna upala koju izazivaju mogu erodirati u krvne žile jednjaka i uzrokovati krvarenje u jednjak.
Ponekad je krvarenje jako i može zahtijevati:
Čirevi na jednjaku zacjeljuju stvaranjem ožiljaka (fibroze). S vremenom se ožiljno tkivo smanjuje i sužava lumen (unutarnju šupljinu) jednjaka. Ovo ožiljno suženje naziva se striktura. Progutana hrana može zaglaviti u jednjaku kada suženje postane dovoljno ozbiljno (obično kada ograniči lumen jednjaka na promjer od jednog centimetra). Ova situacija može zahtijevati endoskopsko uklanjanje zaglavljene hrane. Zatim, da se hrana ne bi lijepila, suženje se mora rastegnuti (proširiti). Štoviše, kako bi se spriječilo ponovno pojavljivanje strikture, refluks se također mora spriječiti.
Dugotrajni i/ili teški GERB uzrokuje promjene u stanicama koje oblažu jednjak u nekih bolesnika. Ove stanice su prekancerozne i mogu, iako obično, postati kancerozne. Ovo stanje se naziva Barrettov jednjak i javlja se u otprilike 10% pacijenata s GERB-om. Tip karcinoma jednjaka povezan s Barrettovim jednjakom (adenokarcinom) je sve učestaliji. Nije jasno zašto neki pacijenti s GERB-om razviju Barrettov jednjak, ali većina ne.
Barrettov jednjak može se vizualno prepoznati u vrijeme endoskopije i potvrditi mikroskopskim pregledom stanica sluznice. Zatim, pacijenti s Barrettovim jednjakom mogu se podvrgnuti periodičnoj nadzornoj endoskopiji s biopsijama iako ne postoji suglasnost o tome koji pacijenti trebaju nadzor. Svrha nadzora je otkriti progresiju od predkanceroznih do više kanceroznih promjena kako bi se moglo započeti liječenje za prevenciju raka. Također se vjeruje da pacijenti s Barrettovim jednjakom trebaju dobiti maksimalan tretman za GERB kako bi se spriječilo daljnje oštećenje jednjaka. Proučavaju se postupci kojima se uklanjaju abnormalne stanice sluznice. Za uklanjanje stanica može se koristiti nekoliko endoskopskih, nekirurških tehnika. Ove tehnike su atraktivne jer ne zahtijevaju operaciju; međutim, postoje povezane s komplikacijama, a dugoročna učinkovitost liječenja još nije utvrđena. Kirurško uklanjanje jednjaka uvijek je opcija.
Mnogi živci su u donjem dijelu jednjaka. Neki od ovih živaca su stimulirani refluksiranom kiselinom, a ta stimulacija rezultira bolom (obično žgaravicom). Ostali živci koji su stimulirani ne proizvode bol. Umjesto toga, oni stimuliraju druge živce koji izazivaju kašalj. Na taj način refluksirana tekućina može uzrokovati kašalj, a da nikada ne dođe do grla! Na sličan način, refluks u donji dio jednjaka može stimulirati živce jednjaka koji se povezuju i mogu stimulirati živce koji idu u pluća. Ti živci u plućima tada mogu uzrokovati sužavanje manjih dišnih cijevi, što rezultira napadom astme.
Iako GERB može uzrokovati kašalj, nije čest uzrok neobjašnjivog kašlja. Iako GERB također može biti uzrok astme, vjerojatnije je da izaziva astmatične napade kod pacijenata koji već imaju astmu. Iako su kronični kašalj i astma uobičajene bolesti, nije jasno koliko su često pogoršani ili uzrokovani GERB-om.
Ako refluksirana tekućina prođe kroz gornji sfinkter jednjaka, može ući u grlo (ždrijelo), pa čak i u govornu kutiju (larinks). Nastala upala može dovesti do upale grla i promuklosti. Kao i kod kašlja i astme, nije jasno koliko je često GERB odgovoran za inače neobjašnjivu upalu grla i larinksa.
Refluksirana tekućina koja prolazi iz grla (ždrijela) u grkljan može ući u pluća (aspiracija). Refluks tekućine u pluća (nazvan aspiracija) često rezultira kašljanjem i gušenjem. Aspiracija se, međutim, također može dogoditi bez pojave ovih simptoma. Sa ili bez ovih simptoma, aspiracija može dovesti do infekcije pluća i dovesti do upale pluća. Ova vrsta upale pluća je ozbiljan problem koji zahtijeva hitno liječenje. Kada aspiracija nije popraćena simptomima, može rezultirati polaganim, progresivnim ožiljcima na plućima (plućna fibroza) što se može vidjeti na rendgenskim snimkama prsnog koša. Vjerojatnije je da će se aspiracija pojaviti noću jer tada procesi (mehanizmi) koji štite od refluksa nisu aktivni, a refleks kašlja koji štiti pluća također nije aktivan.
Grlo komunicira s nosnim prolazima. U male djece dvije mrlje limfnog tkiva, koje se nazivaju adenoidi, nalaze se na mjestu gdje se gornji dio grla spaja s nosnim prolazima. Prolazi iz sinusa i cijevi iz srednjeg uha (Eustahijeve cijevi) otvaraju se u stražnji dio nosnih prolaza u blizini adenoida. Refluksirana tekućina koja ulazi u gornji dio grla može upaliti adenoide i uzrokovati njihovo oticanje. Natečeni adenoidi tada mogu blokirati prolaze iz sinusa i Eustahijeve cijevi. Kada su sinusi i srednje uho zatvorene od nosnih prolaza zbog oticanja adenoida, tekućina se nakuplja unutar njih. Ovo nakupljanje tekućine može dovesti do nelagode u sinusima i ušima. Budući da su adenoidi izraženi kod male djece, a ne kod odraslih, to nakupljanje tekućine u ušima i sinusima viđa se kod djece, a ne kod odraslih.
Postoje različiti postupci, testovi i procjena simptoma (na primjer, žgaravica) za dijagnosticiranje i procjenu pacijenata s GERB-om.
Uobičajeni način na koji se GERB javlja po svom karakterističnom simptomu, žgaravici. Žgaravica se najčešće opisuje kao sub-sternalno pečenje (ispod sredine prsnog koša) koje se javlja nakon jela i često se pogoršava kada ležite. Kako bi potvrdili dijagnozu, liječnici često liječe pacijente lijekovima za suzbijanje proizvodnje kiseline u želucu. Ako se žgaravica tada u velikoj mjeri smanji, dijagnoza GERB-a se smatra potvrđenom. Ovaj pristup postavljanja dijagnoze na temelju odgovora simptoma na liječenje obično se naziva terapijskim ispitivanjem.
Postoje problemi s ovim pristupom. Na primjer, pacijenti koji imaju stanja koja mogu oponašati GERB, posebno čir na dvanaesniku ili želucu (želudac), također mogu stvarno reagirati na takvo liječenje. U ovoj situaciji, ako liječnik pretpostavi da je problem GERB, propustio bi se uzrok ulkusne bolesti, kao što je vrsta infekcije koja se zove Helicobacter pylori (H. pylori ), ili nesteroidni protuupalni lijekovi ili NSAR (na primjer, ibuprofen), također mogu uzrokovati čireve i ta stanja bi se liječila drugačije od GERB-a.
Štoviše, kao i kod svakog liječenja, postoji možda 20% placebo učinka, što znači da će 20% pacijenata odgovoriti na placebo (neaktivnu) pilulu ili, zapravo, na bilo koji tretman. To znači da će 20% pacijenata koji imaju druge simptome osim GERB-a (ili ulkusa) imati smanjenje simptoma nakon liječenja GERB-a. Dakle, na temelju njihovog odgovora na liječenje (terapijsko ispitivanje), ovi će se pacijenti nastaviti liječiti od GERB-a, iako nemaju GERB. Štoviše, pravi uzrok njihovih simptoma neće se tražiti.
Endoskopija gornjeg gastrointestinalnog trakta (također poznata kao ezofago-gastro-duodenoskopija ili EGD) uobičajen je način dijagnosticiranja GERB-a. EGD je postupak u kojem se guta cijev koja sadrži optički sustav za vizualizaciju. Kako cijev napreduje niz gastrointestinalni trakt, može se pregledati sluznica jednjaka, želuca i dvanaesnika.
Jednjak većine pacijenata sa simptomima refluksa izgleda normalno. Stoga u većini bolesnika endoskopija neće pomoći u dijagnozi GERB-a. Međutim, ponekad se sluznica jednjaka čini upaljenom (ezofagitis). Štoviše, ako se uoče erozije (površinske pukotine sluznice jednjaka) ili čirevi (dublje pukotine sluznice), može se pouzdano postaviti dijagnoza GERB-a. Endoskopija će također identificirati nekoliko komplikacija GERB-a, točnije, čireve, strikture i Barrettov jednjak. Također se mogu dobiti biopsije.
Konačno, drugi uobičajeni problemi koji mogu uzrokovati simptome poput GERB-a mogu se dijagnosticirati (na primjer, čirevi, upala ili rak želuca ili dvanaesnika) pomoću EGD-a.
Biopsije jednjaka koje se dobivaju endoskopom ne smatraju se vrlo korisnima za dijagnosticiranje GERB-a. Oni su, međutim, korisni u dijagnosticiranju karcinoma ili uzroka upale jednjaka, osim refluksa kiseline, osobito infekcija. Štoviše, biopsije su jedino sredstvo za dijagnosticiranje staničnih promjena Barrettova jednjaka. U novije vrijeme sugerira se da će čak i kod pacijenata s GERB-om čiji jednjaci izgledaju kao normalni za oko, biopsije pokazuju proširenje prostora između stanica sluznice, što je moguće indikacija oštećenja. Prerano je, međutim, zaključiti da je vidljivost proširenja dovoljno specifična da bi se sa sigurnošću moglo zaključiti da je GERB prisutan.
Prije uvođenja endoskopije, RTG jednjaka (nazvan ezofagram) bio je jedino sredstvo za dijagnosticiranje GERB-a. Pacijenti su progutali barij (kontrastni materijal), a zatim su napravljene rendgenske snimke jednjaka ispunjenog barijem. Problem s ezofagramom bio je u tome što je to bio neosjetljiv test za dijagnosticiranje GERB-a. Odnosno, nije uspio pronaći znakove GERB-a u mnogih pacijenata koji su imali GERB jer su pacijenti imali malo ili nimalo oštećenja sluznice jednjaka. X-zrake su mogle pokazati samo rijetke komplikacije GERB-a, na primjer, čireve i strikture. X-zrake su napuštene kao sredstvo za dijagnosticiranje GERB-a, iako i dalje mogu biti korisne zajedno s endoskopijom u procjeni komplikacija.
Kada GERB zahvaća grlo ili grkljan i uzrokuje simptome kašlja, promuklosti ili upale grla, pacijenti često posjećuju specijaliste za uho, nos i grlo (ENT). ORL specijalist često nalazi znakove upale grla ili grkljana. Iako su bolesti grla ili grkljana obično uzrok upale, ponekad uzrok može biti GERB. U skladu s tim, ORL specijalisti često pokušavaju liječenje suzbijanjem kiseline kako bi potvrdili dijagnozu GERB-a. Ovaj pristup, međutim, ima iste probleme kao što je gore razmotreno, a koji proizlaze iz korištenja odgovora na liječenje za potvrdu GERB-a.
Testiranje kiseline jednjaka smatra se "zlatnim standardom" za dijagnosticiranje GERB-a. Kao što je već spomenuto, refluks kiseline je uobičajen u općoj populaciji. Međutim, pacijenti sa simptomima ili komplikacijama GERB-a imaju refluks više kiseline od osoba bez simptoma ili komplikacija GERB-a. Štoviše, normalne osobe i bolesnici s GERB-om mogu se umjereno dobro razlikovati jedni od drugih po količini vremena u kojem jednjak sadrži kiselinu.
Količina vremena u kojoj jednjak sadrži kiselinu određuje se testom koji se naziva 24-satni pH test jednjaka. (pH je matematički način izražavanja količine kiselosti.) Za ovaj test, mala cjevčica (kateter) prolazi kroz nos i postavlja se u jednjak. Na vrhu katetera nalazi se senzor koji osjeća kiselinu. Drugi kraj katetera izlazi iz nosa, omota se natrag preko uha i spušta se do struka, gdje se pričvršćuje na snimač. Svaki put kada se kiselina vrati u jednjak iz želuca, ona stimulira senzor i snimač bilježi epizodu refluksa. Nakon razdoblja od 20 do 24 sata, kateter se uklanja i analizira se zapis refluksa s rekordera.
Postoje problemi s korištenjem pH testa za dijagnosticiranje GERB-a. Unatoč činjenici da se normalne osobe i bolesnici s GERB-om mogu prilično dobro razdvojiti na temelju pH studija, razdvajanje nije savršeno. Stoga će neki pacijenti s GERB-om imati normalne količine refluksa kiseline, a neki pacijenti bez GERB-a će imati abnormalne količine refluksa kiseline. Za potvrdu prisutnosti GERB-a potrebno je nešto drugo osim pH testa, na primjer, tipični simptomi, odgovor na liječenje ili prisutnost komplikacija GERB-a. GERB se također može pouzdano dijagnosticirati kada epizode žgaravice koreliraju s refluksom kiseline, što pokazuje ispitivanje kiseline.
pH testiranje se koristi u liječenju GERB-a osim samo dijagnosticiranja GERB-a. Na primjer, test može pomoći u određivanju zašto simptomi GERB-a ne reagiraju na liječenje. Možda 10 do 20 posto pacijenata neće imati značajno poboljšanje simptoma liječenjem GERB-a. Ovaj nedostatak odgovora na liječenje mogao bi biti uzrokovan neučinkovitim liječenjem. To znači da lijek ne suzbija na odgovarajući način proizvodnju kiseline u želucu i ne smanjuje refluks kiseline. Alternativno, nedostatak odgovora može se objasniti netočnom dijagnozom GERB-a. U obje ove situacije, pH test može biti vrlo koristan. Ako testiranje otkrije znatan refluks kiseline dok se lijek nastavlja, tada je liječenje neučinkovito i morat će se promijeniti. Ako testiranje otkrije dobru supresiju kiseline s minimalnim refluksom kiseline, dijagnoza GERB-a je vjerojatno pogrešna i potrebno je tražiti druge uzroke simptoma.
pH se također može koristiti za procjenu je li refluks uzrok simptoma (obično žgaravice). Kako bi napravili ovu procjenu, dok se provodi 24-satno ph testiranje, pacijenti bilježe svaki put kada imaju simptome. Zatim, kada se test analizira, može se utvrditi je li se refluks kiseline dogodio u vrijeme simptoma. Ako se refluks dogodio u isto vrijeme kada i simptomi, onda je refluks vjerojatno uzrok simptoma. Ako refluksa nije bilo u vrijeme simptoma, malo je vjerojatno da će refluks biti uzrok simptoma.
Konačno, pH testiranje može se koristiti za procjenu pacijenata prije endoskopskog ili kirurškog liječenja GERB-a. Kao što je gore spomenuto, oko 20% pacijenata imat će smanjenje simptoma iako nemaju GERB (placebo efekt). Prije endoskopskog ili kirurškog liječenja važno je identificirati te pacijente jer vjerojatno neće imati koristi od liječenja. pH studija može se koristiti za identifikaciju ovih pacijenata jer će imati normalne količine refluksa kiseline.
A newer method for prolonged measurement (48 hours) of acid exposure in the esophagus utilizes a small, wireless capsule that is attached to the esophagus just above the LES. The capsule is passed to the lower esophagus by a tube inserted through either the mouth or the nose. After the capsule is attached to the esophagus, the tube is removed. The capsule measures the acid refluxing into the esophagus and transmits this information to a receiver that is worn at the waist. After the study, usually after 48 hours, the information from the receiver is downloaded into a computer and analyzed. The capsule falls off of the esophagus after 3-5 days and is passed in the stool. (The capsule is not reused.)
The advantage of the capsule over standard pH testing is that there is no discomfort from a catheter that passes through the throat and nose. Moreover, with the capsule, patients look normal (they don't have a catheter protruding from their noses) and are more likely to go about their daily activities, for example, go to work, without feeling self-conscious. Because the capsule records for a longer period than the catheter (48 versus 24 hours), more data on acid reflux and symptoms are obtained. Nevertheless, it is not clear whether obtaining additional information is important.
Capsule pH testing is expensive. Sometimes the capsule does not attach to the esophagus or falls off prematurely. For periods of time the receiver may not receive signals from the capsule, and some of the information about reflux of acid may be lost. Occasionally there is pain with swallowing after the capsule has been placed, and the capsule may need to be removed endoscopically. Use of the capsule is an exciting use of new technology although it has its own specific problems.
Esophageal motility testing determines how well the muscles of the esophagus are working. For motility testing, a thin tube (catheter) is passed through a nostril, down the back of the throat, and into the esophagus. On the part of the catheter that is inside the esophagus are sensors that sense pressure. A pressure is generated within the esophagus that is detected by the sensors on the catheter when the muscle of the esophagus contracts. The end of the catheter that protrudes from the nostril is attached to a recorder that records the pressure. During the test, the pressure at rest and the relaxation of the lower esophageal sphincter are evaluated. The patient then swallows sips of water to evaluate the contractions of the esophagus.
Esophageal motility testing has two important uses in evaluating GERD. The first is in evaluating symptoms that do not respond to treatment for GERD since the abnormal function of the esophageal muscle sometimes causes symptoms that resemble the symptoms of GERD. Motility testing can identify some of these abnormalities and lead to a diagnosis of an esophageal motility disorder. The second use is evaluation prior to surgical or endoscopic treatment for GERD. In this situation, the purpose is to identify patients who also have motility disorders of the esophageal muscle. The reason for this is that in patients with motility disorders, some surgeons will modify the type of surgery they perform for GERD.
Gastric emptying studies are studies that determine how well food empties from the stomach. As discussed above, about 20 % of patients with GERD have slow emptying of the stomach that may be contributing to the reflux of acid. For gastric emptying studies, the patient eats a meal that is labeled with a radioactive substance. A sensor that is similar to a Geiger counter is placed over the stomach to measure how quickly the radioactive substance in the meal empties from the stomach.
Information from the emptying study can be useful for managing patients with GERD. For example, if a patient with GERD continues to have symptoms despite treatment with the usual medications, doctors might prescribe other medications that speed-up emptying of the stomach. Alternatively, in conjunction with GERD surgery, they might do a surgical procedure that promotes a more rapid emptying of the stomach. Nevertheless, it is still debated whether a finding of reduced gastric emptying should prompt changes in the surgical treatment of GERD.
Symptoms of nausea, vomiting, and regurgitation may be due either to abnormal gastric emptying or GERD. An evaluation of gastric emptying, therefore, may be useful in identifying patients whose symptoms are due to abnormal emptying of the stomach rather than to GERD.
The acid perfusion (Bernstein) test is used to determine if chest pain is caused by acid reflux. For the acid perfusion test, a thin tube is passed through one nostril, down the back of the throat, and into the middle of the esophagus. A dilute, acid solution and a physiologic salt solution (similar to the fluid that bathes the body's cells) are alternately poured (perfused) through the catheter and into the esophagus. The patient is unaware of which solution is being infused. If the perfusion with acid provokes the patient's usual pain and perfusion of the salt solution produces no pain, it is likely that the patient's pain is caused by acid reflux.
The acid perfusion test, however, is used only rarely. A better test for correlating pain and acid reflux is a 24-hour esophageal pH or pH capsule study during which patients note when they are having pain. It then can be determined from the pH recording if there was an episode of acid reflux at the time of the pain. This is the preferable way of deciding if acid reflux is causing a patient's pain. It does not work well, however, for patients who have infrequent pain, for example every two to three days, which may be missed by a one or two day pH study. In these cases, an acid perfusion test may be reasonable.
One of the simplest treatments for GERD is referred to as life-style changes, a combination of several changes in habit, particularly related to eating.
As discussed above, reflux of acid is more injurious at night than during the day. At night, when individuals are lying down, it is easier for reflux to occur. The reason that it is easier is because gravity is not opposing the reflux, as it does in the upright position during the day. In addition, the lack of an effect of gravity allows the refluxed liquid to travel further up the esophagus and remain in the esophagus longer. These problems can be overcome partially by elevating the upper body in bed. The elevation is accomplished either by putting blocks under the bed's feet at the head of the bed or, more conveniently, by sleeping with the upper body on a foam rubber wedge. These maneuvers raise the esophagus above the stomach and partially restore the effects of gravity. It is important that the upper body and not just the head be elevated. Elevating only the head does not raise the esophagus and fails to restore the effects of gravity.
Elevation of the upper body at night generally is recommended for all patients with GERD. Nevertheless, most patients with GERD have reflux only during the day and elevation at night is of little benefit for them. It is not possible to know for certain which patients will benefit from elevation at night unless acid testing clearly demonstrates night reflux. However, patients who have heartburn, regurgitation, or other symptoms of GERD at night are probably experiencing reflux at night and definitely should elevate their upper body when sleeping. Reflux also occurs less frequently when patients lie on their left rather than their right sides.
Several changes in eating habits can be beneficial in treating GERD. Reflux is worse following meals. This probably is so because the stomach is distended with food at that time and transient relaxations of the lower esophageal sphincter are more frequent. Therefore, smaller and earlier evening meals may reduce the amount of reflux for two reasons. First, the smaller meal results in lesser distention of the stomach. Second, by bedtime, a smaller and earlier meal is more likely to have emptied from the stomach than is a larger one. As a result, reflux is less likely to occur when patients with GERD lie down to sleep.
Certain foods are known to reduce the pressure in the lower esophageal sphincter and thereby promote reflux. These foods should be avoided and include:
Fatty foods (which should be decreased) and smoking (which should be stopped) also reduce the pressure in the sphincter and promote reflux.
In addition, patients with GERD may find that other foods aggravate their symptoms. Examples are spicy or acid-containing foods, like citrus juices, carbonated beverages, and tomato juice. These foods should also be avoided if they provoke symptoms.
One novel approach to the treatment of GERD is chewing gum. Chewing gum stimulates the production of more bicarbonate-containing saliva and increases the rate of swallowing. After the saliva is swallowed, it neutralizes acid in the esophagus. In effect, chewing gum exaggerates one of the normal processes that neutralize acid in the esophagus. It is not clear, however, how effective chewing gum is in treating heartburn. Nevertheless, chewing gum after meals is certainly worth a try.
There is a variety of over-the-counter (for example, antacids and foam barriers) and prescription medications (for example, proton pump inhibitors, histamine antagonists, and promotility drugs) for treating GERD.
Despite the development of potent medications for the treatment of GERD, antacids remain a mainstay of treatment. Antacids neutralize the acid in the stomach so that there is no acid to reflux. The problem with antacids is that their action is brief. They are emptied from the empty stomach quickly, in less than an hour, and the acid then re-accumulates. The best way to take antacids, therefore, is approximately one hour after meals, which is just before the symptoms of reflux begin after a meal. Since the food from meals slows the emptying from the stomach, an antacid taken after a meal stays in the stomach longer and is effective longer. For the same reason, a second dose of antacids approximately two hours after a meal takes advantage of the continuing post-meal slower emptying of the stomach and replenishes the acid-neutralizing capacity within the stomach.
Antacids may be aluminum, magnesium, or calcium-based. Calcium-based antacids (usually calcium carbonate), unlike other antacids, stimulate the release of gastrin from the stomach and duodenum. Gastrin is the hormone that is primarily responsible for the stimulation of acid secretion by the stomach. Therefore, the secretion of acid rebounds after the direct acid-neutralizing effect of the calcium carbonate is exhausted. The rebound is due to the release of gastrin, which results in an overproduction of acid. Theoretically at least, this increased acid is not good for GERD.
Acid rebound, however, is not clinically important. That is, treatment with calcium carbonate is not less effective or safe than treatment with antacids not containing calcium carbonate. Nevertheless, the phenomenon of acid rebound is theoretically harmful. In practice, therefore, calcium-containing antacids such as Tums and Rolaids are not recommended for frequent use. The occasional use of these calcium carbonate-containing antacids, however, is not believed to be harmful. The advantages of calcium carbonate-containing antacids are their low cost, the calcium they add to the diet, and their convenience as compared to liquids.
Aluminum-containing antacids tend to cause constipation, while magnesium-containing antacids tend to cause diarrhea. If diarrhea or constipation becomes a problem, it may be necessary to switch antacids, or use antacids containing both aluminum and magnesium.
Although antacids can neutralize acid, they do so for only a short period. For substantial neutralization of acid throughout the day, antacids would need to be given frequently, at least every hour.
The first medication developed for the more effective and convenient treatment of acid-related diseases, including GERD, was a histamine antagonist, specifically cimetidine (Tagamet). Histamine is an important chemical because it stimulates acid production by the stomach. Released within the wall of the stomach, histamine attaches to receptors (binders) on the stomach's acid-producing cells and stimulates the cells to produce acid. Histamine antagonists work by blocking the receptor for histamine and thereby preventing histamine from stimulating the acid-producing cells. (Histamine antagonists are referred to as H2 antagonists because the specific receptor they block is the histamine type 2 receptor.)
As histamine is particularly important for the stimulation of acid after meals, H2 antagonists are best taken 30 minutes before meals. The reason for this timing is so that the H2 antagonists will be at peak levels in the body after the meal when the stomach is actively producing acid. H2 antagonists also can be taken at bedtime to suppress the nighttime production of acid.
H2 antagonists are very good for relieving the symptoms of GERD, particularly heartburn. However, they are not very good for healing the inflammation (esophagitis) that may accompany GERD. They are used primarily for the treatment of heartburn in GERD that is not associated with inflammation or complications, such as erosions or ulcers, strictures, or Barrett's esophagus.
Three different H2 antagonists are available by prescription, including cimetidine (Tagamet), nizatidine (Axid), and famotidine (Pepcid). Two of these, cimetidine (Tagamet HB) and famotidine (Pepcid AC, Zantac 360) are available over-the-counter (OTC), without the need for a prescription. However, the OTC dosages are lower than those available by prescription.
The second type of drug developed specifically for acid-related diseases, such as GERD, was a proton pump inhibitor (PPI), specifically, omeprazole (Prilosec). A PPI blocks the secretion of acid into the stomach by the acid-secreting cells. The advantage of a PPI over an H2 antagonist is that the PPI shuts off acid production more completely and for a longer period of time. Not only is the PPI good for treating the symptom of heartburn, but it also is good for protecting the esophagus from acid so that esophageal inflammation can heal.
PPIs are used when H2 antagonists do not relieve symptoms adequately or when complications of GERD such as erosions or ulcers, strictures, or Barrett's esophagus exist. Five different PPIs are approved for the treatment of GERD, including omeprazole (Prilosec, Dexilant), lansoprazole (Prevacid), rabeprazole (Aciphex), pantoprazole (Protonix), and esomeprazole (Nexium), and dexlansoprazole (Dexilant). A sixth PPI product consists of a combination of omeprazole and sodium bicarbonate (Zegerid). PPIs (except for Zegerid) are best taken an hour before meals. The reason for this timing is that the PPIs work best when the stomach is most actively producing acid, which occurs after meals. If the PPI is taken before the meal, it is at peak levels in the body after the meal when the acid is being made.
Pro-motility drugs work by stimulating the muscles of the gastrointestinal tract, including the esophagus, stomach, small intestine, and/or colon. One pro-motility drug, metoclopramide (Reglan), is approved for GERD. Pro-motility drugs increase the pressure in the lower esophageal sphincter and strengthen the contractions (peristalsis) of the esophagus. Both effects would be expected to reduce the reflux of acid. However, these effects on the sphincter and esophagus are small. Therefore, it is believed that the primary effect of metoclopramide may be to speed up emptying of the stomach, which also would be expected to reduce reflux.
Pro-motility drugs are most effective when taken 30 minutes before meals and again at bedtime. They are not very effective for treating either the symptoms or complications of GERD. Therefore, the pro-motility agents are reserved either for patients who do not respond to other treatments or are added to enhance other treatments for GERD.
Foam barriers provide a unique form of treatment for GERD. Foam barriers are tablets that are composed of an antacid and a foaming agent. As the tablet disintegrates and reaches the stomach, it turns into foam that floats on top of the liquid contents of the stomach. The foam forms a physical barrier to the reflux of liquid. At the same time, the antacid bound to the foam neutralizes acid that comes into contact with the foam. The tablets are best taken after meals (when the stomach is distended) and when lying down, both times when reflux is more likely to occur. Foam barriers are not often used as the first or only treatment for GERD. Rather, they are added to other drugs for GERD when the other drugs are not adequately effective in relieving symptoms. There is only one foam barrier, which is a combination of aluminum hydroxide gel, magnesium trisilicate, and alginate (Gaviscon).
The drugs described above usually are effective in treating the symptoms and complications of GERD. Nevertheless, sometimes they are not. For example, despite adequate suppression of acid and relief from heartburn, regurgitation, with its potential for complications in the lungs, may still occur. Moreover, the amounts and/or numbers of drugs that are required for satisfactory treatment are sometimes so great that drug treatment is unreasonable. In such situations, surgery can effectively stop reflux.
The surgical procedure that is done to prevent reflux is technically known as fundoplication and is called reflux surgery or anti-reflux surgery. During fundoplication, any hiatal hernial sac is pulled below the diaphragm and stitched there. In addition, the opening in the diaphragm through which the esophagus passes is tightened around the esophagus. Finally, the upper part of the stomach next to the opening of the esophagus into the stomach is wrapped around the lower esophagus to make an artificial lower esophageal sphincter. All of this surgery can be done through an incision in the abdomen (laparotomy) or using a technique called laparoscopy. During laparoscopy, a small viewing device and surgical instruments are passed through several small puncture sites in the abdomen. This procedure avoids the need for a major abdominal incision.
Surgery is very effective at relieving symptoms and treating the complications of GERD. Approximately 80% of patients will have good or excellent relief of their symptoms for at least 5 to 10 years. Nevertheless, many patients who have had surgery will continue to take drugs for reflux. It is not clear whether they take the drugs because they continue to have reflux and symptoms of reflux or if they take them for symptoms that are being caused by problems other than GERD. The most common complication of fundoplication is swallowed food that sticks at the artificial sphincter. Fortunately, the sticking usually is temporary. If it is not transient, endoscopic treatment to stretch (dilate) the artificial sphincter usually will relieve the problem. Only occasionally is it necessary to re-operate to revise the prior surgery.
Very recently, endoscopic techniques for the treatment of GERD have been developed and tested. One type of endoscopic treatment involves suturing (stitching) the area of the lower esophageal sphincter, which essentially tightens the sphincter.
A second type involves the application of radio-frequency waves to the lower part of the esophagus just above the sphincter. The waves cause damage to the tissue beneath the esophageal lining and a scar (fibrosis) forms. The scar shrinks and pulls on the surrounding tissue, thereby tightening the sphincter and the area above it.
A third type of endoscopic treatment involves the injection of materials into the esophageal wall in the area of the LES. The injected material is intended to increase pressure in the LES and thereby prevent reflux. In one treatment the injected material was a polymer. Unfortunately, the injection of polymer led to serious complications, and the material for injection is no longer available. Another treatment involving injection of expandable pellets also was discontinued. Limited information is available about a third type of injection which uses gelatinous polymethylmethacrylate microspheres.
Endoscopic treatment has the advantage of not requiring surgery. It can be performed without hospitalization. Experience with endoscopic techniques is limited. It is not clear how effective they are, especially long-term. Because the effectiveness and the full extent of potential complications of endoscopic techniques are not clear, it is felt generally that endoscopic treatment should only be done as part of experimental trials.
Transient LES relaxations appear to be the most common way in which acid reflux occurs. Although there is an available drug that prevents relaxations (baclofen), it has side effects that are too frequent to be generally useful. Much attention is being directed at the development of drugs that prevent these relaxations without accompanying side effects.
There are several ways to approach the evaluation and management of GERD. The approach depends primarily on the frequency and severity of symptoms, the adequacy of the response to treatment, and the presence of complications.
For infrequent heartburn, the most common symptom of GERD, life-style changes and an occasional antacid may be all that is necessary. If heartburn is frequent, daily non-prescription-strength (over-the-counter) H2 antagonists may be adequate. A foam barrier also can be used with the antacid or H2 antagonist.
If life-style changes and antacids, non-prescription H2 antagonists, and a foam barrier do not adequately relieve heartburn, it is time to see a physician for further evaluation and to consider prescription-strength drugs. The evaluation by the physician should include an assessment for possible complications of GERD based on the presence of such symptoms or findings as:
Clues to the presence of diseases that may mimic GERD, such as gastric or duodenal ulcers and esophageal motility disorders, should be sought.
If there are no symptoms or signs of complications and no suspicion of other diseases, a therapeutic trial of acid suppression with H2 antagonists often is used. If H2 antagonists are not adequately effective, a second trial, with the more potent PPIs, can be given. Sometimes, a trial of treatment begins with a PPI and skips the H2 antagonist. If treatment relieves the symptoms completely, no further evaluation may be necessary and the effective drug, the H2 antagonist or PPI, is continued. As discussed previously, however, there are potential problems with this commonly used approach, and some physicians would recommend a further evaluation for almost all patients they see.
If at the time of evaluation, there are symptoms or signs that suggest complicated GERD or a disease other than GERD or if the relief of symptoms with H2 antagonists or PPIs is not satisfactory, a further evaluation by endoscopy (EGD) definitely should be done.
There are several possible results of endoscopy and each requires a different approach to treatment. If the esophagus is normal and no other diseases are found, the goal of treatment simply is to relieve symptoms. Therefore, prescription strength H2 antagonists or PPIs are appropriate. If damage to the esophagus (esophagitis or ulceration) is found, the goal of treatment is healing the damage. In this case, PPIs are preferred over H2 antagonists because they are more effective for healing.
If complications of GERD, such as stricture or Barrett's esophagus are found, treatment with PPIs also is more appropriate. However, the adequacy of the PPI treatment probably should be evaluated with a 24-hour pH study during treatment with the PPI. (With PPIs, although the amount of acid reflux may be reduced enough to control symptoms, it may still be abnormally high. Therefore, judging the adequacy of suppression of acid reflux by only the response of symptoms to treatment is not satisfactory.) Strictures may also need to be treated by endoscopic dilatation (widening) of the esophageal narrowing. With Barrett's esophagus, periodic endoscopic examination should be done to identify pre-malignant changes in the esophagus.
If symptoms of GERD do not respond to maximum doses of PPI, there are two options for management. The first is to perform 24-hour pH testing to determine whether the PPI is ineffective or if a disease other than GERD is likely to be present. If the PPI is ineffective, a higher dose of PPI may be tried. The second option is to go ahead without 24 hour pH testing and to increase the dose of PPI. Another alternative is to add another drug to the PPI that works in a way that is different from the PPI, for example, a pro-motility drug or a foam barrier. If necessary, all three types of drugs can be used. If there is not a satisfactory response to this maximal treatment, 24 hour pH testing should be done.
Who should consider surgery or, perhaps, an endoscopic treatment trial for GERD? (As mentioned previously, the effectiveness of the recently developed endoscopic treatments remains to be determined.) Patients should consider surgery if they have regurgitation that cannot be controlled with drugs. This recommendation is particularly important if the regurgitation results in infections in the lungs or occurs at night when aspiration into the lungs is more likely. Patients also should consider surgery if they require large doses of PPI or multiple drugs to control their reflux. It is debated whether or not a desire to be free of the need to take life-long drugs to prevent symptoms of GERD is by itself a satisfactory reason for having surgery.
Some physicians - primarily surgeons - recommend that all patients with Barrett's esophagus should have surgery. This recommendation is based on the belief that surgery is more effective than endoscopic surveillance or ablation of the abnormal tissue followed by treatment with acid-suppressing drugs in preventing both the reflux and the cancerous changes in the esophagus. There are no studies, however, demonstrating the superiority of surgery over drugs or ablation for the treatment of GERD and its complications. Moreover, the effectiveness of drug treatment can be monitored with 24 hour pH testing.
One unresolved issue in GERD is the inconsistent relationships among acid reflux, heartburn, and damage to the lining of the esophagus (esophagitis and the complications).
Clearly, we have much to learn about the relationship between acid reflux and esophageal damage, and about the processes (mechanisms) responsible for heartburn. This issue is of more than passing interest. Knowledge of the mechanisms that produce heartburn and esophageal damage raises the possibility of new treatments that would target processes other than acid reflux.
One of the more interesting theories that has been proposed to answer some of these questions involves the reason for pain when acid refluxes. It often is assumed that the pain is caused by irritating acid contacting an inflamed esophageal lining. But the esophageal lining usually is not inflamed. It is possible therefore, that the acid is stimulating the pain nerves within the esophageal wall just beneath the lining. Although this may be the case, a second explanation is supported by the work of one group of scientists. These scientists find that heartburn provoked by acid in the esophagus is associated with contraction of the muscle in the lower esophagus. Perhaps it is the contraction of the muscle that somehow leads to the pain. It also is possible, however, that the contraction is an epiphenomenon, that is, refluxed acid stimulates pain nerves and causes the muscle to contract, but it is not the contraction that causes the pain. More studies will be necessary before the exact mechanism(s) that causes heartburn is clear.
There are potentially injurious agents that can be refluxed other than acid, for example, bile. Until recently it has been impossible or difficult to accurately identify non-acid reflux and, therefore, to study whether or not non-acid reflux is injurious or can cause symptoms.
A new technology allows the accurate determination of non-acid reflux. This technology uses the measurement of impedance changes within the esophagus to identify reflux of liquid, be it acid or non-acid. By combining measurement of impedance and pH it is possible to identify reflux and to tell if the reflux is acid or non-acid. It is too early to know how important non-acid reflux is in causing esophageal damage, symptoms, or complications, but there is little doubt that this new technology will be able to resolve the issues surrounding non-acid reflux.
 Zašto povraćamo kad se razbolimo?
Zašto povraćamo kad se razbolimo?
 Riblji sluz mogao bi biti potencijalni izvor antibiotika
Riblji sluz mogao bi biti potencijalni izvor antibiotika
 Divertikularna bolest i divertikulitis
Divertikularna bolest i divertikulitis
 3 savjeta bez muke kako nahraniti svoju obitelj pravom hranom
3 savjeta bez muke kako nahraniti svoju obitelj pravom hranom
 Crna djeca manje sklona uzimati lijekove za bolove u želucu u hitnoj:studija
Crna djeca manje sklona uzimati lijekove za bolove u želucu u hitnoj:studija
 Kada se trebam brinuti zbog boli kile?
Kada se trebam brinuti zbog boli kile?
 Bubrežni kamenci:simptomi, uzroci i liječenje
Što su bubrežni kamenci? Bubrežni kamenci su male mase soli i minerala koje se stvaraju unutar bubrega i mogu putovati niz mokraćni trakt. Bubrežni kamenci su veličine od samo zrnca do veličine lopt
Bubrežni kamenci:simptomi, uzroci i liječenje
Što su bubrežni kamenci? Bubrežni kamenci su male mase soli i minerala koje se stvaraju unutar bubrega i mogu putovati niz mokraćni trakt. Bubrežni kamenci su veličine od samo zrnca do veličine lopt
 Masna jetra (bezalkoholna masna jetra)
Koje činjenice trebam znati o nealkoholnoj bolesti masne jetre (NASH)? Nealkoholna masna bolest jetre (nealkoholna masna bolest jetre, NAFLD) je nakupljanje abnormalnih količina masti u jetri. Nealk
Masna jetra (bezalkoholna masna jetra)
Koje činjenice trebam znati o nealkoholnoj bolesti masne jetre (NASH)? Nealkoholna masna bolest jetre (nealkoholna masna bolest jetre, NAFLD) je nakupljanje abnormalnih količina masti u jetri. Nealk
 Mogu li jesti pire krumpir 2 dana prije kolonoskopije?
Kolonoskopija je postupak koji se koristi za otkrivanje abnormalnosti u debelom crijevu (debelom crijevu). Dan prije zahvata preporuča se ne jesti krutu ili polukrutu hranu, poput pire krumpira, umaka
Mogu li jesti pire krumpir 2 dana prije kolonoskopije?
Kolonoskopija je postupak koji se koristi za otkrivanje abnormalnosti u debelom crijevu (debelom crijevu). Dan prije zahvata preporuča se ne jesti krutu ili polukrutu hranu, poput pire krumpira, umaka