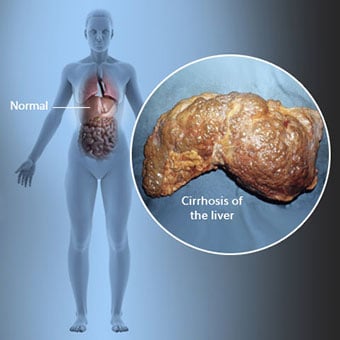
 Ciroza je zaplet bolezni jeter, ki vključuje izgubo jetrnih celic in nepopravljivo brazgotinjenje jeter.
Ciroza je zaplet bolezni jeter, ki vključuje izgubo jetrnih celic in nepopravljivo brazgotinjenje jeter. Posamezniki s cirozo imajo lahko malo ali nič simptomov in znakov bolezni jeter. Nekateri simptomi so lahko nespecifični, to pomeni, da ne kažejo, da so jetra njihov vzrok. Nekateri pogostejši simptomi in znaki ciroze vključujejo:
Posamezniki s cirozo razvijejo tudi simptome in znake zaradi zapletov ciroze.
 Obstaja veliko vzrokov za cirozo, vključno s kemikalijami (kot so alkohol, maščoba in nekatera zdravila), virusi, strupeni kovine in avtoimunska bolezen jeter, pri kateri imunski sistem telesa napada jetra.
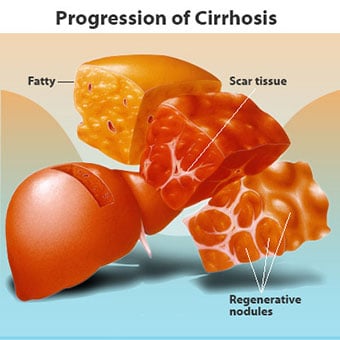
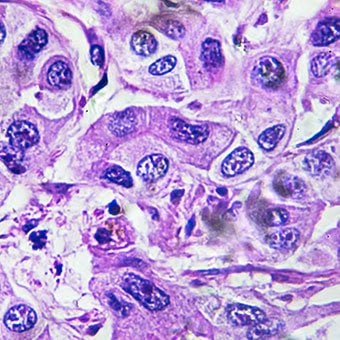
Obstaja veliko vzrokov za cirozo, vključno s kemikalijami (kot so alkohol, maščoba in nekatera zdravila), virusi, strupeni kovine in avtoimunska bolezen jeter, pri kateri imunski sistem telesa napada jetra. Ciroza je zaplet številnih bolezni jeter, za katere je značilna nenormalna struktura in delovanje jeter. Bolezni, ki vodijo v cirozo, to storijo, ker poškodujejo in ubijejo jetrne celice, nato pa vnetje in popravilo, ki je povezano z umirajočimi jetrnimi celicami, povzroči nastanek brazgotin. Jetrne celice, ki ne odmrejo, se množijo, da bi nadomestile celice, ki so umrle. Posledica tega so skupine novonastalih jetrnih celic (regenerativni vozliči) znotraj brazgotinskega tkiva. Obstaja veliko vzrokov za cirozo, vključno s kemikalijami (kot so alkohol, maščobe in nekatera zdravila), virusi, strupenimi kovinami (kot sta železo in baker, ki se kopičita v jetrih kot posledica genetskih bolezni) in avtoimunsko boleznijo jeter, pri kateri imunski sistem telesa napada jetra.
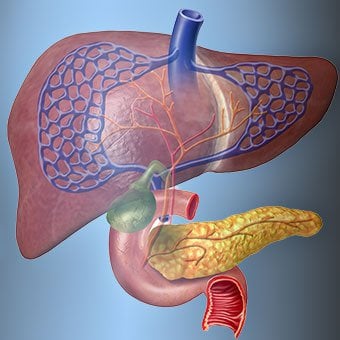
 Odnos jeter in krvi je edinstven.
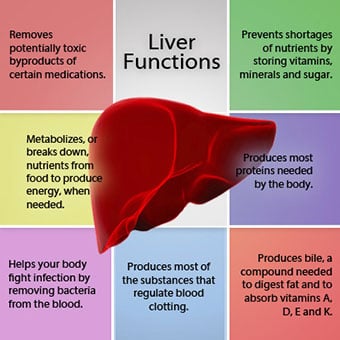
Odnos jeter in krvi je edinstven. Jetra so pomemben organ v telesu. Opravlja številne kritične funkcije, od katerih sta dve proizvajanje snovi, ki jih telo potrebuje, na primer strjevanje beljakovin, ki so potrebne za strjevanje krvi, in odstranjevanje strupenih snovi, ki so lahko škodljive za telo, na primer drog. . Jetra imajo tudi pomembno vlogo pri uravnavanju oskrbe z glukozo (sladkorjem) in lipidi (maščobe), ki jih telo uporablja kot gorivo. Za izvajanje teh kritičnih funkcij morajo jetrne celice normalno delovati in morajo biti v neposredni bližini krvi, saj se snovi, ki jih jetra dodajajo ali odstranijo, s krvjo prenašajo v jetra in iz njih.
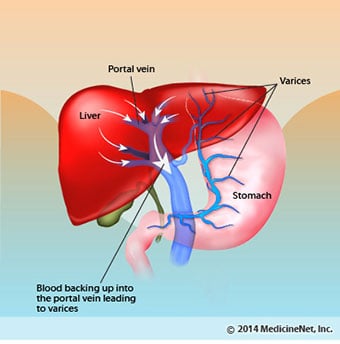
Odnos jeter in krvi je edinstven. Za razliko od večine telesnih organov se jetra po arterijah oskrbuje le z majhno količino krvi. Večina oskrbe jeter s krvjo prihaja iz črevesnih žil, ko se kri vrača v srce. Glavna vena, ki vrača kri iz črevesja, se imenuje portalna vena. Ko portalna vena prehaja skozi jetra, se razpade na vse manjše in manjše vene. Najmanjše žile (imenovane sinusoidi zaradi svoje edinstvene strukture) so v tesnem stiku z jetrnimi celicami. Jetrne celice se vrstijo vzdolž dolžine sinusoidov. Ta tesna povezava med jetrnimi celicami in krvjo iz portalne vene omogoča jetrnim celicam, da odstranijo in dodajo snovi v kri. Ko kri preide skozi sinusoide, se zbira v vedno večjih in večjih venah, ki na koncu tvorijo eno veno, jetrno veno, ki vrača kri v srce.
Pri cirozi se poruši odnos med krvjo in jetrnimi celicami. Čeprav so jetrne celice, ki preživijo ali so na novo oblikovane, lahko sposobne proizvajati in odstraniti snovi iz krvi, nimajo normalnega, intimnega odnosa s krvjo, kar moti sposobnost jetrnih celic, da dodajajo ali odstranijo snovi. iz krvi. Poleg tega brazgotina v cirotičnih jetrih ovira pretok krvi skozi jetra in jetrne celice. Zaradi oviranja pretoka krvi skozi jetra se kri "zadrži" v portalni veni in tlak v portalni veni se poveča, stanje, imenovano portalna hipertenzija. Zaradi ovir za pretok in visokega tlaka v portalni veni kri v portalni veni išče druge žile, v katerih bi se vrnila v srce, vene z nižjim tlakom, ki obidejo jetra. Žal jetra ne morejo dodati ali odstraniti snovi iz krvi, ki jih obide. Kombinacija zmanjšanega števila jetrnih celic, izgube normalnega stika med krvjo, ki teče skozi jetra in jetrne celice, ter krvjo, ki obide jetra, vodi do številnih znakov ciroze.
Drugi razlog za težave, ki jih povzroča ciroza, je moteno razmerje med jetrnimi celicami in kanali, po katerih teče žolč. Žolč je tekočina, ki jo proizvajajo jetrne celice in ima dve pomembni funkciji:pomoč pri prebavi ter odstranjevanje in odstranjevanje strupenih snovi iz telesa. Žolč, ki ga proizvajajo jetrne celice, se izloča v zelo drobne kanale, ki potekajo med jetrnimi celicami, ki obdajajo sinusoide, imenovane kanalčki. Kanalikuli se izlijejo v majhne kanale, ki se nato združijo v vse večje in večje kanale. Vsi kanali se združijo v en kanal, ki vstopi v tanko črevo, kjer lahko pomaga pri prebavi hrane. Hkrati strupene snovi, ki jih vsebuje žolč, vstopijo v črevesje in se nato izločijo z blatom. Pri cirozi so kanalčki nenormalni in razmerje med jetrnimi celicami in kanalički je uničeno, tako kot razmerje med jetrnimi celicami in krvjo v sinusoidih. Posledično jetra ne morejo normalno izločati strupenih snovi in se lahko kopičijo v telesu. V manjši meri se zmanjša tudi prebava v črevesju.
 Pogosti simptomi in znaki ciroze vključujejo zlatenico, utrujenost, šibkost, izgubo apetita, srbenje in lahke modrice.
Pogosti simptomi in znaki ciroze vključujejo zlatenico, utrujenost, šibkost, izgubo apetita, srbenje in lahke modrice. Ljudje s cirozo imajo lahko malo ali nič simptomov in znakov bolezni jeter. Nekateri simptomi so lahko nespecifični in ne kažejo, da so jetra njihov vzrok. Pogosti simptomi in znaki ciroze vključujejo:
Ljudje s cirozo, če jetra razvijejo tudi simptome in znake zaradi zapletov bolezni.
Ciroza sama po sebi je že pozna faza okvare jeter. V zgodnjih fazah bolezni jeter pride do vnetja jeter. Če tega vnetja ne zdravimo, lahko povzroči brazgotinjenje (fibrozo). V tej fazi se jetra še vedno lahko pozdravijo z zdravljenjem.
Če se fibroza jeter ne zdravi, lahko povzroči cirozo. V tej fazi se brazgotinsko tkivo ne more zaceliti, vendar je mogoče preprečiti ali upočasniti napredovanje brazgotine. Ljudje s cirozo, ki imajo znake zapletov, lahko razvijejo končno stopnjo bolezni jeter (ESLD) in edino zdravljenje v tej fazi je presaditev jeter.
 Edem, ascites in zapleti bakterijskega peritonitisa
Edem, ascites in zapleti bakterijskega peritonitisa Ko ciroza jeter postane resna, se ledvicam pošljejo signali, da zadržijo sol in vodo v telesu. Presežek soli in vode se najprej nabere v tkivu pod kožo gležnjev in nog zaradi učinka gravitacije, ko stojite ali sedite. To kopičenje tekočine imenujemo periferni edem ali pitting edem. (Pitting edem se nanaša na dejstvo, da močno pritiskanje konice prsta na gleženj ali nogo z edemom povzroči vdolbino v koži, ki vztraja še nekaj časa po sprostitvi pritiska. Vsaka vrsta pritiska, na primer iz elastičnega traku nogavice , je lahko dovolj, da povzroči izbokline.) Oteklina se pogosto poslabša ob koncu dneva po vstajanju ali sedenju in se lahko zmanjša čez noč, ko ležite. Ker se ciroza poslabša in se zadržuje več soli in vode, se lahko v trebušni votlini nabira tudi tekočina med trebušno steno in trebušnimi organi (imenovani ascites), kar povzroči otekanje trebuha, nelagodje v trebuhu in povečano težo.
Tekočina v trebušni votlini (ascites) je idealno mesto za rast bakterij. Običajno je v trebušni votlini zelo majhna količina tekočine, ki se lahko dobro upre okužbi, bakterije, ki pridejo v trebuh (običajno iz črevesja), pa se ubijejo ali najdejo pot v portalno veno in v jetra, kjer se ubijejo. Pri cirozi se tekočina, ki se nabira v trebuhu, ne more normalno upreti okužbi. Poleg tega več bakterij najde pot iz črevesja v ascites. Verjetno se pojavi okužba v trebuhu in ascitesu, imenovana spontani bakterijski peritonitis ali SBP. SBP je življenjsko nevaren zaplet. Nekateri bolniki s SBP nimajo simptomov, drugi pa imajo zvišano telesno temperaturo, mrzlico, bolečine in občutljivost v trebuhu, drisko in poslabšanje ascitesa.
 Krvavitve in zapleti z vranico
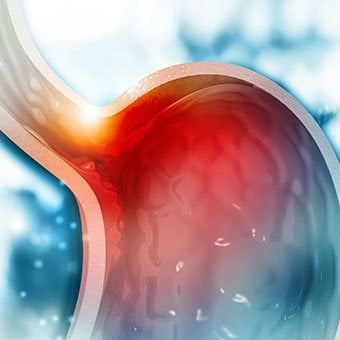
Krvavitve in zapleti z vranico Pri cirotičnih jetrih brazgotina blokira pretok krvi, ki se vrača v srce iz črevesja, in dvigne tlak v portalni veni (portalna hipertenzija). Ko tlak v portalni veni postane dovolj visok, povzroči, da kri teče okoli jeter skozi vene z nižjim tlakom, da doseže srce. Najpogostejše žile, skozi katere kri zaobide jetra, so žile, ki obdajajo spodnji del požiralnika in zgornji del želodca.
Zaradi povečanega pretoka krvi in posledičnega povečanja tlaka se žile v spodnjem požiralniku in zgornjem delu želodca razširijo in jih nato imenujemo krčne žile požiralnika in želodca; višji kot je portalni tlak, večje so krčne žile in večja je verjetnost, da bo bolnik krvavel iz krčnih žil v požiralnik ali želodec.
Krvavitev iz krčnih žil je huda in brez takojšnjega zdravljenja je lahko usodna. Simptomi krvavitve iz krčnih žil vključujejo bruhanje krvi (lahko je videti kot rdeča kri, pomešana s strdki ali "kavno usedlino"), črno in katranasto blato zaradi sprememb v krvi, ko prehaja skozi črevo (melena), in ortostatsko omotica ali omedlevica (povzročena zaradi padca krvnega tlaka, zlasti pri vstajanju iz ležečega položaja).
Redko se lahko pojavijo krvavitve iz krčnih žil, ki nastanejo drugje v črevesju, na primer v debelem črevesu. Bolniki, ki so hospitalizirani zaradi aktivno krvavečih krčnih žil požiralnika, imajo veliko tveganje za razvoj spontanega bakterijskega peritonitisa, čeprav razlogi za to še niso razumljeni.
Vranica običajno deluje kot filter za odstranjevanje starejših rdečih krvnih celic, belih krvnih celic in trombocitov (majhni delci, pomembni za strjevanje krvi). Kri, ki odteka iz vranice, se pridruži krvi v portalni veni iz črevesja. Ker pri cirozi narašča tlak v portalni veni, ta vse bolj blokira pretok krvi iz vranice. Kri se "nabira" v vranici in vranica nabrekne v velikosti, stanje, ki se imenuje splenomegalija. Včasih je vranica tako povečana, da povzroča bolečine v trebuhu.
Ko se vranica poveča, filtrira vse več krvnih celic in trombocitov, dokler se njihovo število v krvi ne zmanjša. Hipersplenizem je izraz, ki se uporablja za opis tega stanja in je povezan z nizkim številom rdečih krvnih celic (anemija), nizkim številom belih krvnih celic (levkopenija) in/ali nizkim številom trombocitov (trombocitopenija). Anemija lahko povzroči šibkost, levkopenija lahko povzroči okužbe, trombocitopenija pa lahko poslabša strjevanje krvi in povzroči podaljšano krvavitev
 Jetrni (jetrni) zapleti
Jetrni (jetrni) zapleti Ciroza zaradi katerega koli vzroka poveča tveganje za primarni rak jeter (hepatocelularni karcinom). Primarni se nanaša na dejstvo, da tumor izvira iz jeter. Sekundarni rak jeter je tisti, ki izvira drugje v telesu in se širi (metastazira) v jetra.
Najpogostejši simptomi in znaki primarnega raka jeter so bolečine v trebuhu in otekanje, povečana jetra, izguba telesne mase in zvišana telesna temperatura. Poleg tega lahko rak jeter proizvaja in sprošča številne snovi, vključno s tistimi, ki povzročajo povečano število rdečih krvnih celic (eritrocitoza), nizek krvni sladkor (hipoglikemija) in visok kalcij v krvi (hiperkalcemija).
Nekatere beljakovine v hrani, ki se izognejo prebavi in absorpciji, uporabljajo bakterije, ki so običajno prisotne v črevesju. Medtem ko beljakovine uporabljajo za lastne namene, bakterije proizvajajo snovi, ki jih sproščajo v črevesje, da se nato absorbirajo v telo. Nekatere od teh snovi, kot je amoniak, imajo lahko toksične učinke na možgane. Običajno se te strupene snovi prenašajo iz črevesja v portalni veni v jetra, kjer se odstranijo iz krvi in razstrupljajo.
Ko je ciroza prisotna, jetrne celice ne morejo normalno delovati, ker so poškodovane ali ker so izgubile normalno razmerje s krvjo. Poleg tega nekaj krvi v portalni veni zaobide jetra skozi druge vene. Posledica teh nepravilnosti je, da jetrne celice ne morejo odstraniti strupenih snovi, temveč se kopičijo v krvi.
Ko se strupene snovi v krvi kopičijo v zadostni količini, pride do motenj v delovanju možganov, kar se imenuje jetrna encefalopatija. Spanje podnevi in ne ponoči (sprememba običajnega vzorca spanja) je zgodnji simptom jetrne encefalopatije. Drugi simptomi vključujejo razdražljivost, nezmožnost koncentracije ali izvajanja izračunov, izgubo spomina, zmedenost ali depresivno raven zavesti. Na koncu huda jetrna encefalopatija povzroči komo in smrt.
Zaradi strupenih snovi so možgani bolnikov s cirozo zelo občutljivi na zdravila, ki jih jetra običajno filtrirajo in razstrupljajo. Morda bo treba zmanjšati odmerke številnih zdravil, da se prepreči kopičenje strupenih snovi pri cirozi, zlasti pomirjeval in zdravil, ki se uporabljajo za spodbujanje spanja. Druga možnost je, da se uporabljajo zdravila, ki jih jetra ni treba razstrupljati ali izločiti iz telesa, na primer zdravila, ki jih izločajo ledvice.
Pri bolnikih s poslabšanjem ciroze se lahko razvije hepatorenalni sindrom. Ta sindrom je resen zaplet, pri katerem se zmanjša delovanje ledvic. Gre za funkcionalno težavo v ledvicah, kar pomeni, da ledvice niso fizične poškodbe. Namesto tega je zmanjšana funkcija posledica sprememb v načinu pretoka krvi skozi same ledvice. Hepatorenalni sindrom je opredeljen kot progresivna odpoved ledvic, da očistijo snovi iz krvi in proizvedejo ustrezne količine urina, medtem ko se ohranijo druge pomembne funkcije ledvic, kot je zadrževanje soli. Če se delovanje jeter izboljša ali bolniku s hepatorenalnim sindromom presadijo zdrava jetra, ledvice običajno spet začnejo normalno delovati. To nakazuje, da je zmanjšano delovanje ledvic posledica bodisi kopičenja strupenih snovi v krvi bodisi nenormalnega delovanja jeter, ko jetra odpovedujejo. Obstajata dve vrsti hepatorenalnega sindroma. Ena vrsta se pojavlja postopoma v mesecih. Drugi se pojavi hitro v tednu ali dveh.
Redko lahko nekateri bolniki z napredovalo cirozo razvijejo hepatopulmonalni sindrom. Ti bolniki imajo lahko težave z dihanjem, ker nekateri hormoni, ki se sproščajo pri napredovali cirozi, povzročajo nenormalno delovanje pljuč. Osnovna težava v pljučih je, da skozi majhne krvne žile v pljučih, ki so v stiku z alveoli (zračnimi vrečkami) pljuč, teče premalo krvi. Kri, ki teče skozi pljuča, se premika okoli alveolov in ne more pobrati dovolj kisika iz zraka v alveolah. Posledica tega je, da bolnik občuti težko dihanje, zlasti pri naporu.
 There are 12 common causes of cirrhosis.
There are 12 common causes of cirrhosis. Common causes of cirrhosis of the liver include:
Less common causes of cirrhosis include:
In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
 Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis.
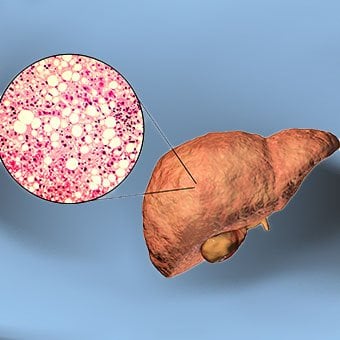
Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis. Alcohol is a very common cause of cirrhosis, particularly in the Western world. Chronic, high levels of alcohol consumption injure liver cells. Thirty percent of individuals who drink daily at least eight to sixteen ounces of hard liquor or the equivalent for fifteen or more years will develop cirrhosis. Alcohol causes a range of liver diseases, which include simple and uncomplicated fatty liver (steatosis), more serious fatty liver with inflammation (steatohepatitis or alcoholic hepatitis), and cirrhosis.
Nonalcoholic fatty liver disease (NAFLD) refers to a wide spectrum of liver diseases that, like alcoholic liver disease, range from simple steatosis, to nonalcoholic steatohepatitis (NASH), to cirrhosis. All stages of NAFLD have in common the accumulation of fat in liver cells. The term nonalcoholic is used because NAFLD occurs in individuals who do not consume excessive amounts of alcohol, yet in many respects the microscopic picture of NAFLD is similar to what can be seen in liver disease that is due to excessive alcohol. NAFLD is associated with a condition called insulin resistance, which, in turn, is associated with metabolic syndrome and diabetes mellitus type 2. Obesity is the main cause of insulin resistance, metabolic syndrome, and type 2 diabetes. NAFLD is the most common liver disease in the United States and is responsible for up to 25% of all liver disease. The number of livers transplanted for NAFLD-related cirrhosis is on the rise. Public health officials are worried that the current epidemic of obesity will dramatically increase the development of NAFLD and cirrhosis in the population.
 Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women.
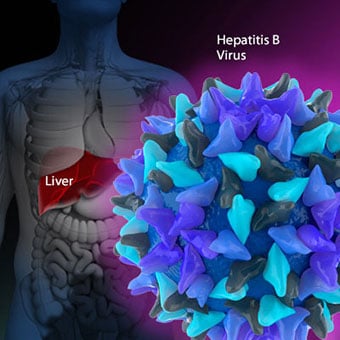
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. Chronic viral hepatitis is a condition in which hepatitis B or hepatitis C virus infects the liver for years. Most patients with viral hepatitis will not develop chronic hepatitis and cirrhosis. The majority of patients infected with hepatitis A recover completely within weeks, without developing chronic infection. In contrast, some patients infected with hepatitis B virus and most patients infected with hepatitis C virus develop chronic hepatitis, which, in turn, causes progressive liver damage and leads to cirrhosis, and, sometimes, liver cancers.
Autoimmune hepatitis is a liver disease found more commonly in women that is caused by an abnormality of the immune system. The abnormal immune activity in autoimmune hepatitis causes progressive inflammation and destruction of liver cells (hepatocytes), leading ultimately to cirrhosis.
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. The abnormal immunity in PBC causes chronic inflammation and destruction of the small bile ducts within the liver. The bile ducts are passages within the liver through which bile travels to the intestine. Bile is a fluid produced by the liver that contains substances required for digestion and absorption of fat in the intestine, as well as other compounds that are waste products, such as the pigment bilirubin. (Bilirubin is produced by the breakdown of hemoglobin from old red blood cells.). Along with the gallbladder, the bile ducts make up the biliary tract. In PBC, the destruction of the small bile ducts blocks the normal flow of bile into the intestine. As the inflammation continues to destroy more of the bile ducts, it also spreads to destroy nearby liver cells. As the destruction of the hepatocytes proceeds, scar tissue (fibrosis) forms and spreads throughout the areas of destruction. The combined effects of progressive inflammation, scarring, and the toxic effects of accumulating waste products culminates in cirrhosis.
Primary sclerosing cholangitis (PSC) is an uncommon disease frequently found in patients with Crohn's disease and ulcerative colitis. In PSC, the large bile ducts outside of the liver become inflamed, narrowed, and obstructed. Obstruction to the flow of bile leads to infections of the bile ducts and jaundice, eventually causing cirrhosis. In some patients, injury to the bile ducts (usually because of surgery) also can cause obstruction and cirrhosis of the liver.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. Inherited (genetic) disorders that result in the accumulation of toxic substances in the liver, which leads to tissue damage and cirrhosis. Examples include the abnormal accumulation of iron (hemochromatosis) or copper (Wilson disease). In hemochromatosis, patients inherit a tendency to absorb an excessive amount of iron from food. Over time, iron accumulation in different organs throughout the body causes cirrhosis, arthritis, heart muscle damage leading to heart failure, and testicular dysfunction causing loss of sexual drive. Treatment is aimed at preventing damage to organs by removing iron from the body through phlebotomy (removing blood). In Wilson disease, there is an inherited abnormality in one of the proteins that control copper in the body. Over time, copper accumulates in the liver, eyes, and brain. Cirrhosis, tremor, psychiatric disturbances, and other neurological difficulties occur if the condition is not treated early. Treatment is with oral medication, which increases the amount of copper that is eliminated from the body in the urine.
Cryptogenic cirrhosis (cirrhosis due to unidentified causes) is a common reason for liver transplantation. It is termed called cryptogenic cirrhosis because for many years doctors have been being unable to explain why a proportion of patients developed cirrhosis. Doctors now believe that cryptogenic cirrhosis is due to NASH (nonalcoholic steatohepatitis) caused by long-standing obesity, type 2 diabetes, and insulin resistance. The fat in the liver of patients with NASH is believed to disappear with the onset of cirrhosis, and this has made it difficult for doctors to make the connection between NASH and cryptogenic cirrhosis for a long time. One important clue that NASH leads to cryptogenic cirrhosis is the finding of a high occurrence of NASH in the new livers of patients undergoing liver transplant for cryptogenic cirrhosis. Finally, a study from France suggests that patients with NASH have a similar risk of developing cirrhosis as patients with long-standing infection with hepatitis C virus. (See discussion that follows.) However, the progression to cirrhosis from NASH is thought to be slow and the diagnosis of cirrhosis typically is made in people in their sixties.
Infants can be born without bile ducts (biliary atresia) and ultimately develop cirrhosis. Other infants are born lacking vital enzymes for controlling sugars that lead to the accumulation of sugars and cirrhosis. On rare occasions, the absence of a specific enzyme can cause cirrhosis and scarring of the lung (alpha-1 antitrypsin deficiency).
Less common causes of cirrhosis include unusual reactions to some drugs and prolonged exposure to toxins, as well as chronic heart failure (cardiac cirrhosis). In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. The single best test for diagnosing cirrhosis is a biopsy of the liver. Liver biopsies carry a small risk for serious complications, and biopsy often is reserved for those patients in whom the diagnosis of the type of liver disease or the presence of cirrhosis is not clear. The history, physical examination, or routine testing may suggest the possibility of cirrhosis. If cirrhosis is present, other tests can be used to determine the severity of the cirrhosis and the presence of complications. Tests also may be used to diagnose the underlying disease that is causing the cirrhosis. Examples of how doctors diagnose and evaluate cirrhosis are:
 There are four types of treatment of cirrhosis.
There are four types of treatment of cirrhosis. Treatment of cirrhosis includes
Consume a balanced diet and one multivitamin daily. Patients with PBC with impaired absorption of fat-soluble vitamins may need additional vitamins D and K.
Avoid drugs (including alcohol) that cause liver damage. All patients with cirrhosis should avoid alcohol. Most patients with alcohol-induced cirrhosis experience an improvement in liver function with abstinence from alcohol. Even patients with chronic hepatitis B and C can substantially reduce liver damage and slow the progression towards cirrhosis with abstinence from alcohol.
Avoid nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen). Patients with cirrhosis can experience worsening of liver and kidney function with NSAIDs.
Eradicate hepatitis B and hepatitis C virus by using anti-viral medications. Not all patients with cirrhosis due to chronic viral hepatitis are candidates for drug treatment. Some patients may experience serious deterioration in liver function and/or intolerable side effects during treatment. Thus, decisions to treat viral hepatitis have to be individualized, after consulting with doctors experienced in treating liver diseases (hepatologists).
Remove blood from patients with hemochromatosis to reduce the levels of iron and prevent further damage to the liver. In Wilson's disease, medications can be used to increase the excretion of copper in the urine to reduce the levels of copper in the body and prevent further damage to the liver.
Suppress the immune system with drugs such as prednisone and azathioprine (Imuran) to decrease inflammation of the liver in autoimmune hepatitis.
Treat patients with PBC with a bile acid preparation, ursodeoxycholic acid (UDCA), also called ursodiol (Actigall). Results of an analysis that combined the results from several clinical trials showed that UDCA increased survival among PBC patients during 4 years of therapy. The development of portal hypertension also was reduced by the UDCA. It is important to note that despite producing clear benefits, UDCA treatment primarily retards progression and does not cure PBC. Other medications such as colchicine and methotrexate also may have benefits in subsets of patients with PBC.
Immunize patients with cirrhosis against infection with hepatitis A and B to prevent a serious deterioration in liver. There are currently no vaccines available for immunizing against hepatitis C.
 Treatment for edema, ascites, and hypersplenism complications.
Treatment for edema, ascites, and hypersplenism complications. Retaining salt and water can lead to swelling of the ankles and legs (edema) or abdomen (ascites) in patients with cirrhosis. Doctors often advise patients with cirrhosis to restrict dietary salt (sodium) and fluid to decrease edema and ascites. The amount of salt in the diet usually is restricted to 2 grams per day and fluid to 1.2 liters per day. In most patients with cirrhosis, salt and fluid restriction is not enough and diuretics have to be added.
Diuretics are medications that work in the kidneys to promote the elimination of salt and water into the urine. A combination of the diuretics spironolactone (Aldactone) and furosemide (Lasix) can reduce or eliminate the edema and ascites in most patients. During treatment with diuretics, it is important to monitor the function of the kidneys by measuring blood levels of blood urea nitrogen (BUN) and creatinine to determine if too much diuretic is being used. Too much diuretic can lead to kidney dysfunction that is reflected in elevations of the BUN and creatinine levels in the blood.
Sometimes, when the diuretics do not work (in which case the ascites is said to be refractory), a long needle or catheter is used to draw out the ascitic fluid directly from the abdomen, a procedure called abdominal paracentesis. It is common to withdraw large amounts (liters) of fluid from the abdomen when the ascites is causing painful abdominal distension and/or difficulty breathing because it limits the movement of the diaphragms.
Another treatment for refractory ascites is a procedure called transjugular intravenous portosystemic shunting (TIPS).
The spleen normally acts as a filter to remove older red blood cells, white blood cells, and platelets (small particles important for the clotting of blood). The blood that drains from the spleen joins the blood in the portal vein from the intestines. As the pressure in the portal vein rises in cirrhosis, it increasingly blocks the flow of blood from the spleen. The blood "backs-up," accumulating in the spleen, and the spleen swells in size, a condition referred to as splenomegaly. Sometimes, the spleen is so enlarged it causes abdominal pain.
As the spleen enlarges, it filters out more and more of the blood cells and platelets until their numbers in the blood are reduced. Hypersplenism is the term used to describe this condition, and it is associated with a low red blood cell count (anemia), low white blood cell count (leukopenia), and/or a low platelet count (thrombocytopenia). Anemia can cause weakness, leucopenia can lead to infections, and thrombocytopenia can impair the clotting of blood and result in prolonged bleeding.
 Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding.
Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. If large varices develop in the esophagus or upper stomach, patients with cirrhosis are at risk for serious bleeding due to rupture of these varices. Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. Treatments include medications and procedures to decrease the pressure in the portal vein and procedures to destroy the varices.
 Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose.
Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Patients with an abnormal sleep cycle, impaired thinking, odd behavior, or other signs of hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Dietary protein is restricted because it is a source of toxic compounds that cause hepatic encephalopathy. Lactulose, which is a liquid, traps toxic compounds in the colon so they cannot be absorbed into the bloodstream, and thus cause encephalopathy. Lactulose is converted to lactic acid in the colon, and the acidic environment that results is believed to trap the toxic compounds produced by the bacteria. To be sure adequate lactulose is present in the colon at all times, the patient should adjust the dose to produce 2 to 3 semiformed bowel movements a day. Lactulose is a laxative, and the effectiveness of treatment can be judged by loosening or increasing the frequency of stools. Rifaximin (Xifaxan) is an antibiotic taken orally that is not absorbed into the body but rather remains in the intestines. It is the preferred mode of treatment of hepatic encephalopathy. Antibiotics work by suppressing the bacteria that produce the toxic compounds in the colon.
 Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics.
Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics. Patients suspected of having spontaneous bacterial peritonitis usually will undergo paracentesis. The fluid that is removed is examined for white blood cells and cultured for bacteria. Culturing involves inoculating a sample of the ascites into a bottle of nutrient-rich fluid that encourages the growth of bacteria, thus facilitating the identification of even small numbers of bacteria. Blood and urine samples also are often obtained for culturing because many patients with spontaneous bacterial peritonitis also will have infections in their blood and urine. Many doctors believe the infection may have begun in the blood and the urine and spread to the ascitic fluid to cause spontaneous bacterial peritonitis. Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics such as cefotaxime (Claforan). Patients usually treated with antibiotics include:
Spontaneous bacterial peritonitis is a serious infection. It often occurs in patients with advanced cirrhosis whose immune systems are weak, but with modern antibiotics and early detection and treatment, the prognosis of recovering from an episode of spontaneous bacterial peritonitis is good.
In some patients, oral antibiotics (norfloxacin [Noroxin] or sulfamethoxazole and trimethoprim [Bactrim]) can be prescribed to prevent spontaneous bacterial peritonitis. Not all patients with cirrhosis and ascites should be treated with antibiotics to prevent spontaneous bacterial peritonitis, but some patients are at high risk for developing spontaneous bacterial peritonitis and warrant preventive treatment.
 The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases. Several types of liver disease that cause cirrhosis (such as hepatitis B and C) are associated with a high incidence of liver cancer. It is useful to screen for liver cancer in patients with cirrhosis, as early surgical treatment or transplantation of the liver can cure the patient of cancer. The difficulty is that the methods available for screening are only partially effective, identifying at best only half of patients at a curable stage of their cancer. Despite the partial effectiveness of screening, most patients with cirrhosis, particularly hepatitis B and C, are screened yearly or every six months with ultrasound examination of the liver and measurements of cancer-produced proteins in the blood, for example, alpha-fetoprotein.
Cirrhosis is irreversible. Liver function usually gradually worsens despite treatment, and complications of cirrhosis increase and become difficult to treat. When cirrhosis is far advanced liver transplantation often is the only option for treatment. Recent advances in surgical transplantation and medications to prevent infection and rejection of the transplanted liver have greatly improved survival after transplantation. On average, more than 80% of patients who receive transplants are alive after five years. Not everyone with cirrhosis is a candidate for transplantation. Furthermore, there is a shortage of livers to transplant, and they're usually is a long (months to years) wait before a liver for transplanting becomes available. Measures to slow the progression of liver disease, and treat and prevent complications of cirrhosis are vitally important.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
Progress in the management and prevention of cirrhosis continues. Research is ongoing to determine the mechanism of scar formation in the liver and how this process of scarring can be interrupted or even reversed. Newer and better treatments for viral liver disease are being developed to prevent the progression to cirrhosis. Prevention of viral hepatitis by vaccination, which is available for hepatitis B, is being developed for hepatitis C. Treatments for the complications of cirrhosis are being developed or revised, and tested continually. Finally, research is being directed at identifying new proteins in the blood that can detect liver cancer early or predict which patients will develop liver cancer.
 Vaša neodtujljiva pravica do dobrega zdravja in sreče
Vaša neodtujljiva pravica do dobrega zdravja in sreče
 Bakterijske spremembe v črevesju vplivajo na rezultate zdravljenja lupusa v nosečnosti
Bakterijske spremembe v črevesju vplivajo na rezultate zdravljenja lupusa v nosečnosti
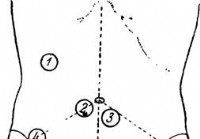 Raziskava želodca - Diagnoza akutnega trebuha
Raziskava želodca - Diagnoza akutnega trebuha
 Koliko laktoze lahko prenesem?
Koliko laktoze lahko prenesem?
 Kako mi je hrana spremenila življenje:premagovanje utrujenosti, depresije in prebavnih težav
Kako mi je hrana spremenila življenje:premagovanje utrujenosti, depresije in prebavnih težav
 Vse, kar morate vedeti o žolčnih kamnih
Vse, kar morate vedeti o žolčnih kamnih
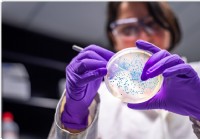 Močan mikrobiom v zgodnjem življenju je povezan z manj okužbami dihal
V različnih delih človeškega telesa, vključno z nosom, obstajajo kolonije mikroskopskih bakterij usta, črevesje, in pljuča. Skupaj, te bakterije so znane kot telesna mikrobiota. Študije so pokazale,
Močan mikrobiom v zgodnjem življenju je povezan z manj okužbami dihal
V različnih delih človeškega telesa, vključno z nosom, obstajajo kolonije mikroskopskih bakterij usta, črevesje, in pljuča. Skupaj, te bakterije so znane kot telesna mikrobiota. Študije so pokazale,
 Kako poskrbeti za zdravje prebave:redno uživanje fermentiranega mleka lahko izboljša blage prebavne simptome
Občasni gastrointestinalni simptomi so pogosti pri sicer zdravi populaciji. Večina simptomov se odziva na spremembe v prehrani, verjetno s spremembami v črevesni mikrobioti. Dokazi kažejo, da ima preh
Kako poskrbeti za zdravje prebave:redno uživanje fermentiranega mleka lahko izboljša blage prebavne simptome
Občasni gastrointestinalni simptomi so pogosti pri sicer zdravi populaciji. Večina simptomov se odziva na spremembe v prehrani, verjetno s spremembami v črevesni mikrobioti. Dokazi kažejo, da ima preh
 Nasveti za zdrav pristop k novemu letu
Povzetek:Izboljšajte svoje prebavno zdravje to novo leto tako, da vzpostavite zdrave navade, kot so opustitev kajenja, redna vadba in uživanje več vlaknin. Običajna tradicija zvonjenja v novem letu
Nasveti za zdrav pristop k novemu letu
Povzetek:Izboljšajte svoje prebavno zdravje to novo leto tako, da vzpostavite zdrave navade, kot so opustitev kajenja, redna vadba in uživanje več vlaknin. Običajna tradicija zvonjenja v novem letu