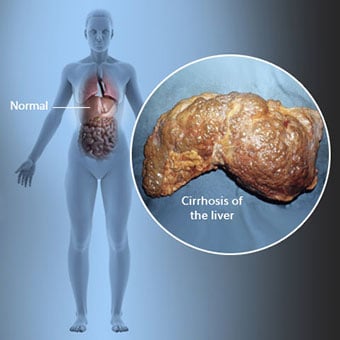
 Ciroza je komplikacija bolesti jetre koja uključuje gubitak stanica jetre i nepovratno stvaranje ožiljaka na jetri.
Ciroza je komplikacija bolesti jetre koja uključuje gubitak stanica jetre i nepovratno stvaranje ožiljaka na jetri. Osobe s cirozom mogu imati malo ili nimalo simptoma i znakova bolesti jetre. Neki od simptoma mogu biti nespecifični, odnosno ne upućuju na to da im je jetra uzrok. Neki od češćih simptoma i znakova ciroze su:
Osobe s cirozom također razvijaju simptome i znakove komplikacija ciroze.
 Postoje mnogi uzroci ciroze, uključujući kemikalije (kao što su alkohol, masti i određeni lijekovi), viruse, toksične metali, te autoimuna bolest jetre u kojoj imunološki sustav tijela napada jetru.
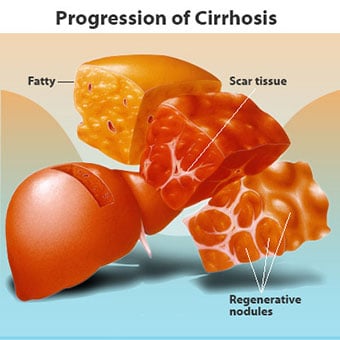
Postoje mnogi uzroci ciroze, uključujući kemikalije (kao što su alkohol, masti i određeni lijekovi), viruse, toksične metali, te autoimuna bolest jetre u kojoj imunološki sustav tijela napada jetru. Ciroza je komplikacija mnogih bolesti jetre koje karakterizira abnormalna struktura i funkcija jetre. Bolesti koje dovode do ciroze to čine jer ozljeđuju i ubijaju stanice jetre, nakon čega upala i popravak koji je povezan s umirućim stanicama jetre uzrokuje stvaranje ožiljnog tkiva. Stanice jetre koje ne umiru množe se u pokušaju da nadomjeste stanice koje su umrle. To rezultira nakupinama novonastalih stanica jetre (regenerativnih čvorova) unutar ožiljnog tkiva. Postoje mnogi uzroci ciroze, uključujući kemikalije (kao što su alkohol, masnoće i određeni lijekovi), viruse, otrovne metale (kao što su željezo i bakar koji se nakupljaju u jetri kao posljedica genetskih bolesti) i autoimunu bolest jetre u kojoj imunološki sustav tijela napada jetru.
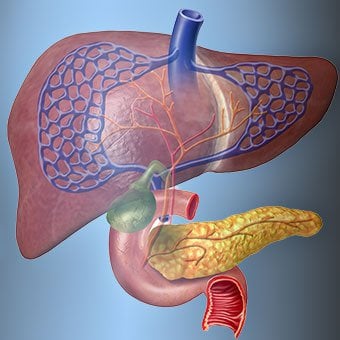
 Odnos jetre i krvi je jedinstven.
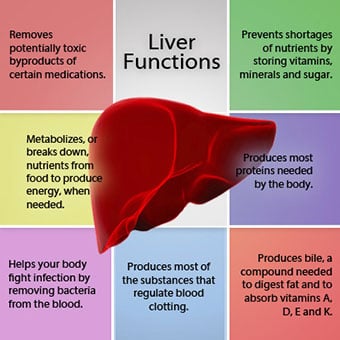
Odnos jetre i krvi je jedinstven. Jetra je važan organ u tijelu. Obavlja mnoge kritične funkcije, od kojih su dvije stvaranje tvari potrebnih tijelu, na primjer, zgrušavanje proteina koji su potrebni za zgrušavanje krvi i uklanjanje otrovnih tvari koje mogu biti štetne za tijelo, na primjer, kao što su lijekovi . Jetra također ima važnu ulogu u reguliranju opskrbe glukozom (šećerom) i lipidima (masti) koje tijelo koristi kao gorivo. Da bi obavljale ove kritične funkcije, stanice jetre moraju raditi normalno i moraju biti u neposrednoj blizini krvi jer se tvari koje jetra dodaje ili uklanja krvlju transportuje u jetru i iz jetre.
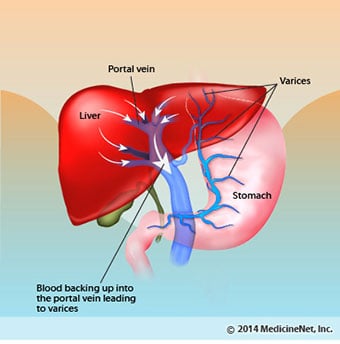
Odnos jetre i krvi je jedinstven. Za razliku od većine organa u tijelu, samo mala količina krvi se opskrbljuje jetrom putem arterija. Većina opskrbe jetre krvlju dolazi iz crijevnih vena dok se krv vraća u srce. Glavna vena koja vraća krv iz crijeva naziva se portalna vena. Kako portalna vena prolazi kroz jetru, ona se raspada na sve manje i manje vene. Najsitnije vene (nazvane sinusoidi zbog svoje jedinstvene strukture) u bliskom su kontaktu sa stanicama jetre. Stanice jetre nižu se duž dužine sinusoida. Ovaj bliski odnos između stanica jetre i krvi iz portalne vene omogućuje stanicama jetre da uklone i dodaju tvari u krv. Nakon što krv prođe kroz sinusoide, skuplja se u sve veće i veće vene koje u konačnici tvore jednu venu, jetrenu venu, koja vraća krv u srce.
Kod ciroze se razara odnos između krvi i jetrenih stanica. Iako stanice jetre koje prežive ili su novoformirane mogu proizvoditi i uklanjati tvari iz krvi, one nemaju normalan, prisan odnos s krvlju, što ometa sposobnost stanica jetre da dodaju ili uklanjaju tvari. od krvi. Osim toga, ožiljci unutar cirotične jetre ometaju protok krvi kroz jetru i do jetrenih stanica. Kao rezultat ometanja protoka krvi kroz jetru, krv se "nalazi" u portalnoj veni, a tlak u portalnoj veni raste, stanje koje se naziva portalna hipertenzija. Zbog opstrukcije protoka i visokog tlaka u portalnoj veni, krv u portalnoj veni traži druge vene u kojima se vraća u srce, vene s nižim tlakom koje zaobilaze jetru. Nažalost, jetra nije u stanju dodati ili ukloniti tvari iz krvi koje je zaobilaze. To je kombinacija smanjenog broja jetrenih stanica, gubitka normalnog kontakta između krvi koja prolazi kroz jetru i jetrenih stanica i krvi koja zaobilazi jetru koja dovodi do mnogih znakova ciroze.
Drugi razlog za probleme uzrokovane cirozom je poremećen odnos između stanica jetre i kanala kroz koje teče žuč. Žuč je tekućina koju proizvode jetrene stanice koja ima dvije važne funkcije:pomaže u probavi te uklanja i eliminira otrovne tvari iz tijela. Žuč koju proizvode jetrene stanice izlučuje se u vrlo sićušne kanale koji prolaze između jetrenih stanica koje oblažu sinusoide, zvane kanalići. Kanalikuli se prazne u male kanaliće koji se zatim spajaju u sve veće i veće kanale. Svi kanali se spajaju u jedan kanal koji ulazi u tanko crijevo gdje može pomoći u probavi hrane. Istodobno, otrovne tvari sadržane u žuči ulaze u crijevo, a zatim se eliminiraju stolicom. Kod ciroze, kanalići su abnormalni i odnos između stanica jetre i kanalića je uništen, baš kao i odnos između stanica jetre i krvi u sinusoidima. Kao rezultat toga, jetra nije u stanju normalno eliminirati otrovne tvari i one se mogu nakupljati u tijelu. U manjoj mjeri, probava u crijevima je također smanjena.
 Uobičajeni simptomi i znakovi ciroze uključuju žuticu, umor, slabost, gubitak apetita, svrbež i lako stvaranje modrica.
Uobičajeni simptomi i znakovi ciroze uključuju žuticu, umor, slabost, gubitak apetita, svrbež i lako stvaranje modrica. Osobe s cirozom mogu imati malo ili nimalo simptoma i znakova bolesti jetre. Neki od simptoma mogu biti nespecifični i ne sugeriraju da je jetra njihov uzrok. Uobičajeni simptomi i znakovi ciroze uključuju:
Osobe s cirozom ako jetra također razvije simptome i znakove komplikacija bolesti.
Ciroza je sama po sebi već kasni stadij oštećenja jetre. U ranim fazama bolesti jetre dolazi do upale jetre. Ako se ova upala ne liječi može dovesti do ožiljaka (fibroze). U ovoj fazi još je moguće da se jetra liječi liječenjem.
Ako se fibroza jetre ne liječi, može rezultirati cirozom. U ovoj fazi, ožiljno tkivo ne može zacijeliti, ali se napredovanje ožiljaka može spriječiti ili usporiti. Ljudi s cirozom koji imaju znakove komplikacija mogu razviti završnu bolest jetre (ESLD), a jedini način liječenja u ovoj fazi je transplantacija jetre.
 Edem, ascites i komplikacije bakterijskog peritonitisa
Edem, ascites i komplikacije bakterijskog peritonitisa Kako ciroza jetre postaje teška, bubrezima se šalju signali da zadrže sol i vodu u tijelu. Višak soli i vode prvo se nakuplja u tkivu ispod kože gležnjeva i nogu zbog djelovanja gravitacije kada stojite ili sjedite. Ovo nakupljanje tekućine naziva se periferni edem ili pitting edem. (Pitting edem odnosi se na činjenicu da čvrsto pritiskanje vrha prsta na gležanj ili nogu s edemom uzrokuje udubljenje na koži koje traje neko vrijeme nakon otpuštanja pritiska. Bilo koja vrsta pritiska, poput elastične trake čarape , može biti dovoljno da izazove pojavu jamica.) Oteklina je često jača na kraju dana nakon stajanja ili sjedenja i može se smanjiti tijekom noći kada ležite. Kako se ciroza pogoršava i zadržava se više soli i vode, tekućina se također može nakupljati u trbušnoj šupljini između trbušne stijenke i trbušnih organa (tzv. ascites) što uzrokuje oticanje trbuha, nelagodu u trbuhu i povećanje težine.
Tekućina u trbušnoj šupljini (ascites) savršeno je mjesto za razvoj bakterija. Normalno, trbušna šupljina sadrži vrlo malu količinu tekućine koja se može dobro oduprijeti infekciji, a bakterije koje uđu u abdomen (obično iz crijeva) stradaju ili pronađu put do portalne vene i do jetre gdje su ubijene. Kod ciroze tekućina koja se skuplja u abdomenu ne može se normalno oduprijeti infekciji. Osim toga, više bakterija pronalazi put iz crijeva u ascites. Vjerojatno će doći do infekcije unutar abdomena i ascitesa, nazvane spontani bakterijski peritonitis ili SBP. SBP je komplikacija opasna po život. Neki pacijenti sa SBP nemaju simptome, dok drugi imaju groznicu, zimicu, bol i osjetljivost u trbuhu, proljev i pogoršanje ascitesa.
 Krvarenje i komplikacije slezene
Krvarenje i komplikacije slezene U cirotičnoj jetri, ožiljno tkivo blokira protok krvi koja se vraća u srce iz crijeva i podiže tlak u portalnoj veni (portalna hipertenzija). Kada tlak u portalnoj veni postane dovoljno visok, uzrokuje da krv teče oko jetre kroz vene s nižim tlakom kako bi stigla do srca. Najčešće vene kroz koje krv zaobilazi jetru su vene koje oblažu donji dio jednjaka i gornji dio želuca.
Kao rezultat povećanog protoka krvi i rezultirajućeg povećanja tlaka, vene u donjem dijelu jednjaka i gornjem dijelu želuca se šire i tada se nazivaju varikozi jednjaka i želuca; što je veći portalni tlak, veće su varikoze i veća je vjerojatnost da će pacijent krvariti iz varikoziteta u jednjak ili želudac.
Krvarenje iz varikoziteta je teško i bez hitnog liječenja može biti smrtonosno. Simptomi krvarenja iz varikoziteta uključuju povraćanje krvi (može izgledati kao crvena krv pomiješana s ugrušcima ili "talogom od kave"), izlučivanje crne i katranaste stolice zbog promjena u krvi dok prolazi kroz crijeva (melena) i ortostatski vrtoglavica ili nesvjestica (uzrokovane padom krvnog tlaka, osobito kada se ustanete iz ležećeg položaja).
Rijetko se može pojaviti krvarenje iz varikoziteta koji se formiraju na drugim mjestima u crijevima, na primjer, debelo crijevo. Pacijenti hospitalizirani zbog aktivnog krvarenja varikoziteta jednjaka imaju visok rizik od razvoja spontanog bakterijskog peritonitisa, iako razlozi za to još nisu razjašnjeni.
Slezena normalno djeluje kao filter za uklanjanje starijih crvenih krvnih stanica, bijelih krvnih stanica i trombocita (male čestice važne za zgrušavanje krvi). Krv koja istječe iz slezene pridružuje se krvi u portalnoj veni iz crijeva. Kako tlak u portalnoj veni raste kod ciroze, ona sve više blokira protok krvi iz slezene. Krv se "podržava", nakuplja se u slezeni, a slezena nabubri u veličini, stanje koje se naziva splenomegalija. Ponekad je slezena toliko povećana da uzrokuje bolove u trbuhu.
Kako se slezena povećava, ona filtrira sve više krvnih stanica i trombocita dok se njihov broj u krvi ne smanji. Hipersplenizam je izraz koji se koristi za opisivanje ovog stanja, a povezan je s niskim brojem crvenih krvnih stanica (anemija), niskim brojem bijelih krvnih stanica (leukopenija) i/ili niskim brojem trombocita (trombocitopenija). Anemija može uzrokovati slabost, leukopenija može dovesti do infekcija, a trombocitopenija može narušiti zgrušavanje krvi i rezultirati produljenim krvarenjem
 Komplikacije jetre (jetre)
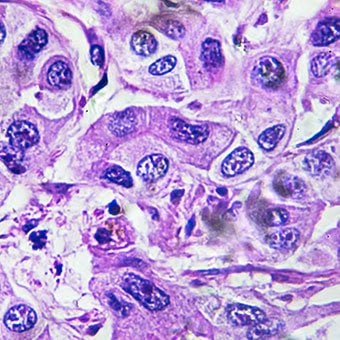
Komplikacije jetre (jetre) Ciroza zbog bilo kojeg uzroka povećava rizik od primarnog karcinoma jetre (hepatocelularni karcinom). Primarni se odnosi na činjenicu da tumor potječe iz jetre. Sekundarni karcinom jetre je onaj koji nastaje negdje drugdje u tijelu i širi se (metastazira) u jetru.
Najčešći simptomi i znakovi primarnog karcinoma jetre su bol i oteklina u trbuhu, povećana jetra, gubitak težine i groznica. Osim toga, karcinom jetre može proizvoditi i oslobađati brojne tvari, uključujući one koje uzrokuju povećanje broja crvenih krvnih stanica (eritrocitoza), nisku razinu šećera u krvi (hipoglikemija) i visoku razinu kalcija u krvi (hiperkalcemiju).
Dio proteina u hrani koji izbjegne probavu i apsorpciju koriste bakterije koje su normalno prisutne u crijevima. Dok koriste protein u vlastite svrhe, bakterije stvaraju tvari koje otpuštaju u crijeva da bi se potom apsorbirale u tijelo. Neke od tih tvari, kao što je amonijak, mogu imati toksične učinke na mozak. Obično se te otrovne tvari prenose iz crijeva u portalnoj veni u jetru gdje se uklanjaju iz krvi i detoksificiraju.
Kada je prisutna ciroza, stanice jetre ne mogu normalno funkcionirati jer su oštećene ili zato što su izgubile normalan odnos s krvlju. Osim toga, dio krvi u portalnoj veni zaobilazi jetru kroz druge vene. Rezultat ovih abnormalnosti je da stanice jetre ne mogu ukloniti otrovne tvari, već se akumuliraju u krvi.
Kada se otrovne tvari akumuliraju dovoljno u krvi, funkcija mozga je oštećena, stanje koje se naziva hepatična encefalopatija. Spavanje tijekom dana, a ne noću (preokret od normalnog obrasca spavanja) rani je simptom jetrene encefalopatije. Ostali simptomi uključuju razdražljivost, nemogućnost koncentracije ili izračunavanja, gubitak pamćenja, zbunjenost ili depresivnu razinu svijesti. U konačnici, teška jetrena encefalopatija uzrokuje komu i smrt.
Otrovne tvari također čine mozak pacijenata s cirozom vrlo osjetljivim na lijekove koje jetra normalno filtrira i detoksificira. Doze mnogih lijekova možda će se morati smanjiti kako bi se izbjeglo nakupljanje toksičnih tvari u cirozi, osobito sedativa i lijekova koji se koriste za poticanje sna. Alternativno, mogu se koristiti lijekovi koji se ne moraju detoksificirati ili eliminirati iz tijela putem jetre, kao što su lijekovi koji se eliminiraju putem bubrega.
Bolesnici s pogoršanjem ciroze mogu razviti hepatorenalni sindrom. Ovaj sindrom je ozbiljna komplikacija u kojoj je smanjena funkcija bubrega. To je funkcionalni problem u bubrezima, što znači da nema fizičkog oštećenja bubrega. Umjesto toga, smanjena funkcija je posljedica promjena u načinu na koji krv teče kroz same bubrege. Hepatorenalni sindrom definira se kao progresivno zatajenje bubrega da očiste tvari iz krvi i proizvedu odgovarajuću količinu urina dok se druge važne funkcije bubrega, poput zadržavanja soli, održavaju. Ako se funkcija jetre poboljša ili se zdrava jetra transplantira u bolesnika s hepatorenalnim sindromom, bubrezi obično ponovno počinju normalno raditi. To sugerira da je smanjena funkcija bubrega rezultat ili nakupljanja otrovnih tvari u krvi ili abnormalne funkcije jetre kada jetra zataji. Postoje dvije vrste hepatorenalnog sindroma. Jedna se vrsta javlja postupno tijekom mjeseci. Drugi se događa brzo tijekom tjedan ili dva.
Rijetko, neki bolesnici s uznapredovalom cirozom mogu razviti hepatopulmonalni sindrom. Ovi pacijenti mogu osjetiti poteškoće s disanjem jer određeni hormoni koji se oslobađaju u uznapredovaloj cirozi uzrokuju nenormalan rad pluća. Osnovni problem u plućima je što ne teče dovoljno krvi kroz male krvne žile u plućima koje su u kontaktu s alveolama (zračnim vrećicama) pluća. Krv koja teče kroz pluća skitira se oko alveola i ne može pokupiti dovoljno kisika iz zraka u alveolama. Kao rezultat toga, pacijent osjeća kratak dah, osobito pri naporu.
 Postoji 12 uobičajenih uzroka ciroze.
Postoji 12 uobičajenih uzroka ciroze. Uobičajeni uzroci of cirrhosis of the liver include:
Less common causes of cirrhosis include:
In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
 Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis.
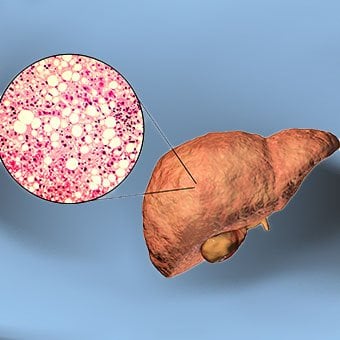
Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis. Alcohol is a very common cause of cirrhosis, particularly in the Western world. Chronic, high levels of alcohol consumption injure liver cells. Thirty percent of individuals who drink daily at least eight to sixteen ounces of hard liquor or the equivalent for fifteen or more years will develop cirrhosis. Alcohol causes a range of liver diseases, which include simple and uncomplicated fatty liver (steatosis), more serious fatty liver with inflammation (steatohepatitis or alcoholic hepatitis), and cirrhosis.
Nonalcoholic fatty liver disease (NAFLD) refers to a wide spectrum of liver diseases that, like alcoholic liver disease, range from simple steatosis, to nonalcoholic steatohepatitis (NASH), to cirrhosis. All stages of NAFLD have in common the accumulation of fat in liver cells. The term nonalcoholic is used because NAFLD occurs in individuals who do not consume excessive amounts of alcohol, yet in many respects the microscopic picture of NAFLD is similar to what can be seen in liver disease that is due to excessive alcohol. NAFLD is associated with a condition called insulin resistance, which, in turn, is associated with metabolic syndrome and diabetes mellitus type 2. Obesity is the main cause of insulin resistance, metabolic syndrome, and type 2 diabetes. NAFLD is the most common liver disease in the United States and is responsible for up to 25% of all liver disease. The number of livers transplanted for NAFLD-related cirrhosis is on the rise. Public health officials are worried that the current epidemic of obesity will dramatically increase the development of NAFLD and cirrhosis in the population.
 Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women.
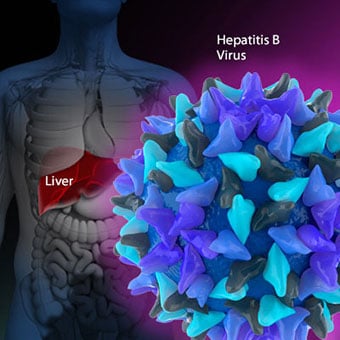
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. Chronic viral hepatitis is a condition in which hepatitis B or hepatitis C virus infects the liver for years. Most patients with viral hepatitis will not develop chronic hepatitis and cirrhosis. The majority of patients infected with hepatitis A recover completely within weeks, without developing chronic infection. In contrast, some patients infected with hepatitis B virus and most patients infected with hepatitis C virus develop chronic hepatitis, which, in turn, causes progressive liver damage and leads to cirrhosis, and, sometimes, liver cancers.
Autoimmune hepatitis is a liver disease found more commonly in women that is caused by an abnormality of the immune system. The abnormal immune activity in autoimmune hepatitis causes progressive inflammation and destruction of liver cells (hepatocytes), leading ultimately to cirrhosis.
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. The abnormal immunity in PBC causes chronic inflammation and destruction of the small bile ducts within the liver. The bile ducts are passages within the liver through which bile travels to the intestine. Bile is a fluid produced by the liver that contains substances required for digestion and absorption of fat in the intestine, as well as other compounds that are waste products, such as the pigment bilirubin. (Bilirubin is produced by the breakdown of hemoglobin from old red blood cells.). Along with the gallbladder, the bile ducts make up the biliary tract. In PBC, the destruction of the small bile ducts blocks the normal flow of bile into the intestine. As the inflammation continues to destroy more of the bile ducts, it also spreads to destroy nearby liver cells. As the destruction of the hepatocytes proceeds, scar tissue (fibrosis) forms and spreads throughout the areas of destruction. The combined effects of progressive inflammation, scarring, and the toxic effects of accumulating waste products culminates in cirrhosis.
Primary sclerosing cholangitis (PSC) is an uncommon disease frequently found in patients with Crohn's disease and ulcerative colitis. In PSC, the large bile ducts outside of the liver become inflamed, narrowed, and obstructed. Obstruction to the flow of bile leads to infections of the bile ducts and jaundice, eventually causing cirrhosis. In some patients, injury to the bile ducts (usually because of surgery) also can cause obstruction and cirrhosis of the liver.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. Inherited (genetic) disorders that result in the accumulation of toxic substances in the liver, which leads to tissue damage and cirrhosis. Examples include the abnormal accumulation of iron (hemochromatosis) or copper (Wilson disease). In hemochromatosis, patients inherit a tendency to absorb an excessive amount of iron from food. Over time, iron accumulation in different organs throughout the body causes cirrhosis, arthritis, heart muscle damage leading to heart failure, and testicular dysfunction causing loss of sexual drive. Treatment is aimed at preventing damage to organs by removing iron from the body through phlebotomy (removing blood). In Wilson disease, there is an inherited abnormality in one of the proteins that control copper in the body. Over time, copper accumulates in the liver, eyes, and brain. Cirrhosis, tremor, psychiatric disturbances, and other neurological difficulties occur if the condition is not treated early. Treatment is with oral medication, which increases the amount of copper that is eliminated from the body in the urine.
Cryptogenic cirrhosis (cirrhosis due to unidentified causes) is a common reason for liver transplantation. It is termed called cryptogenic cirrhosis because for many years doctors have been being unable to explain why a proportion of patients developed cirrhosis. Doctors now believe that cryptogenic cirrhosis is due to NASH (nonalcoholic steatohepatitis) caused by long-standing obesity, type 2 diabetes, and insulin resistance. The fat in the liver of patients with NASH is believed to disappear with the onset of cirrhosis, and this has made it difficult for doctors to make the connection between NASH and cryptogenic cirrhosis for a long time. One important clue that NASH leads to cryptogenic cirrhosis is the finding of a high occurrence of NASH in the new livers of patients undergoing liver transplant for cryptogenic cirrhosis. Finally, a study from France suggests that patients with NASH have a similar risk of developing cirrhosis as patients with long-standing infection with hepatitis C virus. (See discussion that follows.) However, the progression to cirrhosis from NASH is thought to be slow and the diagnosis of cirrhosis typically is made in people in their sixties.
Infants can be born without bile ducts (biliary atresia) and ultimately develop cirrhosis. Other infants are born lacking vital enzymes for controlling sugars that lead to the accumulation of sugars and cirrhosis. On rare occasions, the absence of a specific enzyme can cause cirrhosis and scarring of the lung (alpha-1 antitrypsin deficiency).
Less common causes of cirrhosis include unusual reactions to some drugs and prolonged exposure to toxins, as well as chronic heart failure (cardiac cirrhosis). In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. The single best test for diagnosing cirrhosis is a biopsy of the liver. Liver biopsies carry a small risk for serious complications, and biopsy often is reserved for those patients in whom the diagnosis of the type of liver disease or the presence of cirrhosis is not clear. The history, physical examination, or routine testing may suggest the possibility of cirrhosis. If cirrhosis is present, other tests can be used to determine the severity of the cirrhosis and the presence of complications. Tests also may be used to diagnose the underlying disease that is causing the cirrhosis. Examples of how doctors diagnose and evaluate cirrhosis are:
 There are four types of treatment of cirrhosis.
There are four types of treatment of cirrhosis. Treatment of cirrhosis includes
Consume a balanced diet and one multivitamin daily. Patients with PBC with impaired absorption of fat-soluble vitamins may need additional vitamins D and K.
Avoid drugs (including alcohol) that cause liver damage. All patients with cirrhosis should avoid alcohol. Most patients with alcohol-induced cirrhosis experience an improvement in liver function with abstinence from alcohol. Even patients with chronic hepatitis B and C can substantially reduce liver damage and slow the progression towards cirrhosis with abstinence from alcohol.
Avoid nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen). Patients with cirrhosis can experience worsening of liver and kidney function with NSAIDs.
Eradicate hepatitis B and hepatitis C virus by using anti-viral medications. Not all patients with cirrhosis due to chronic viral hepatitis are candidates for drug treatment. Some patients may experience serious deterioration in liver function and/or intolerable side effects during treatment. Thus, decisions to treat viral hepatitis have to be individualized, after consulting with doctors experienced in treating liver diseases (hepatologists).
Remove blood from patients with hemochromatosis to reduce the levels of iron and prevent further damage to the liver. In Wilson's disease, medications can be used to increase the excretion of copper in the urine to reduce the levels of copper in the body and prevent further damage to the liver.
Suppress the immune system with drugs such as prednisone and azathioprine (Imuran) to decrease inflammation of the liver in autoimmune hepatitis.
Treat patients with PBC with a bile acid preparation, ursodeoxycholic acid (UDCA), also called ursodiol (Actigall). Results of an analysis that combined the results from several clinical trials showed that UDCA increased survival among PBC patients during 4 years of therapy. The development of portal hypertension also was reduced by the UDCA. It is important to note that despite producing clear benefits, UDCA treatment primarily retards progression and does not cure PBC. Other medications such as colchicine and methotrexate also may have benefits in subsets of patients with PBC.
Immunize patients with cirrhosis against infection with hepatitis A and B to prevent a serious deterioration in liver. There are currently no vaccines available for immunizing against hepatitis C.
 Treatment for edema, ascites, and hypersplenism complications.
Treatment for edema, ascites, and hypersplenism complications. Retaining salt and water can lead to swelling of the ankles and legs (edema) or abdomen (ascites) in patients with cirrhosis. Doctors often advise patients with cirrhosis to restrict dietary salt (sodium) and fluid to decrease edema and ascites. The amount of salt in the diet usually is restricted to 2 grams per day and fluid to 1.2 liters per day. In most patients with cirrhosis, salt and fluid restriction is not enough and diuretics have to be added.
Diuretics are medications that work in the kidneys to promote the elimination of salt and water into the urine. A combination of the diuretics spironolactone (Aldactone) and furosemide (Lasix) can reduce or eliminate the edema and ascites in most patients. During treatment with diuretics, it is important to monitor the function of the kidneys by measuring blood levels of blood urea nitrogen (BUN) and creatinine to determine if too much diuretic is being used. Too much diuretic can lead to kidney dysfunction that is reflected in elevations of the BUN and creatinine levels in the blood.
Sometimes, when the diuretics do not work (in which case the ascites is said to be refractory), a long needle or catheter is used to draw out the ascitic fluid directly from the abdomen, a procedure called abdominal paracentesis. It is common to withdraw large amounts (liters) of fluid from the abdomen when the ascites is causing painful abdominal distension and/or difficulty breathing because it limits the movement of the diaphragms.
Another treatment for refractory ascites is a procedure called transjugular intravenous portosystemic shunting (TIPS).
The spleen normally acts as a filter to remove older red blood cells, white blood cells, and platelets (small particles important for the clotting of blood). The blood that drains from the spleen joins the blood in the portal vein from the intestines. As the pressure in the portal vein rises in cirrhosis, it increasingly blocks the flow of blood from the spleen. The blood "backs-up," accumulating in the spleen, and the spleen swells in size, a condition referred to as splenomegaly. Sometimes, the spleen is so enlarged it causes abdominal pain.
As the spleen enlarges, it filters out more and more of the blood cells and platelets until their numbers in the blood are reduced. Hypersplenism is the term used to describe this condition, and it is associated with a low red blood cell count (anemia), low white blood cell count (leukopenia), and/or a low platelet count (thrombocytopenia). Anemia can cause weakness, leucopenia can lead to infections, and thrombocytopenia can impair the clotting of blood and result in prolonged bleeding.
 Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding.
Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. If large varices develop in the esophagus or upper stomach, patients with cirrhosis are at risk for serious bleeding due to rupture of these varices. Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. Treatments include medications and procedures to decrease the pressure in the portal vein and procedures to destroy the varices.
 Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose.
Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Patients with an abnormal sleep cycle, impaired thinking, odd behavior, or other signs of hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Dietary protein is restricted because it is a source of toxic compounds that cause hepatic encephalopathy. Lactulose, which is a liquid, traps toxic compounds in the colon so they cannot be absorbed into the bloodstream, and thus cause encephalopathy. Lactulose is converted to lactic acid in the colon, and the acidic environment that results is believed to trap the toxic compounds produced by the bacteria. To be sure adequate lactulose is present in the colon at all times, the patient should adjust the dose to produce 2 to 3 semiformed bowel movements a day. Lactulose is a laxative, and the effectiveness of treatment can be judged by loosening or increasing the frequency of stools. Rifaximin (Xifaxan) is an antibiotic taken orally that is not absorbed into the body but rather remains in the intestines. It is the preferred mode of treatment of hepatic encephalopathy. Antibiotics work by suppressing the bacteria that produce the toxic compounds in the colon.
 Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics.
Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics. Patients suspected of having spontaneous bacterial peritonitis usually will undergo paracentesis. The fluid that is removed is examined for white blood cells and cultured for bacteria. Culturing involves inoculating a sample of the ascites into a bottle of nutrient-rich fluid that encourages the growth of bacteria, thus facilitating the identification of even small numbers of bacteria. Blood and urine samples also are often obtained for culturing because many patients with spontaneous bacterial peritonitis also will have infections in their blood and urine. Many doctors believe the infection may have begun in the blood and the urine and spread to the ascitic fluid to cause spontaneous bacterial peritonitis. Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics such as cefotaxime (Claforan). Patients usually treated with antibiotics include:
Spontaneous bacterial peritonitis is a serious infection. It often occurs in patients with advanced cirrhosis whose immune systems are weak, but with modern antibiotics and early detection and treatment, the prognosis of recovering from an episode of spontaneous bacterial peritonitis is good.
In some patients, oral antibiotics (norfloxacin [Noroxin] or sulfamethoxazole and trimethoprim [Bactrim]) can be prescribed to prevent spontaneous bacterial peritonitis. Not all patients with cirrhosis and ascites should be treated with antibiotics to prevent spontaneous bacterial peritonitis, but some patients are at high risk for developing spontaneous bacterial peritonitis and warrant preventive treatment.
 The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases. Several types of liver disease that cause cirrhosis (such as hepatitis B and C) are associated with a high incidence of liver cancer. It is useful to screen for liver cancer in patients with cirrhosis, as early surgical treatment or transplantation of the liver can cure the patient of cancer. The difficulty is that the methods available for screening are only partially effective, identifying at best only half of patients at a curable stage of their cancer. Despite the partial effectiveness of screening, most patients with cirrhosis, particularly hepatitis B and C, are screened yearly or every six months with ultrasound examination of the liver and measurements of cancer-produced proteins in the blood, for example, alpha-fetoprotein.
Cirrhosis is irreversible. Liver function usually gradually worsens despite treatment, and complications of cirrhosis increase and become difficult to treat. When cirrhosis is far advanced liver transplantation often is the only option for treatment. Recent advances in surgical transplantation and medications to prevent infection and rejection of the transplanted liver have greatly improved survival after transplantation. On average, more than 80% of patients who receive transplants are alive after five years. Not everyone with cirrhosis is a candidate for transplantation. Furthermore, there is a shortage of livers to transplant, and they're usually is a long (months to years) wait before a liver for transplanting becomes available. Measures to slow the progression of liver disease, and treat and prevent complications of cirrhosis are vitally important.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
Progress in the management and prevention of cirrhosis continues. Research is ongoing to determine the mechanism of scar formation in the liver and how this process of scarring can be interrupted or even reversed. Newer and better treatments for viral liver disease are being developed to prevent the progression to cirrhosis. Prevention of viral hepatitis by vaccination, which is available for hepatitis B, is being developed for hepatitis C. Treatments for the complications of cirrhosis are being developed or revised, and tested continually. Finally, research is being directed at identifying new proteins in the blood that can detect liver cancer early or predict which patients will develop liver cancer.
 Neželjeni učinci Libraxa
Librax je lijek koji se koristi za opuštanje mišića u crijevima i mokraćnom mjehuru. To je jedan od vrsta lijekova koji se nazivaju benzodiazepini. Librax je kombinacija dva lijeka, klordiazepoksida i
Neželjeni učinci Libraxa
Librax je lijek koji se koristi za opuštanje mišića u crijevima i mokraćnom mjehuru. To je jedan od vrsta lijekova koji se nazivaju benzodiazepini. Librax je kombinacija dva lijeka, klordiazepoksida i
 Butternut tikva Mac n’ Cheese
Ponekad moj petogodišnji sin dođe kući iz škole i traži da “jede hranu koju imaju druga djeca”. Zato dajem sve od sebe da improviziram, kao kad sam mu napravio sendviče s jabukama. Ponekad druga djec
Butternut tikva Mac n’ Cheese
Ponekad moj petogodišnji sin dođe kući iz škole i traži da “jede hranu koju imaju druga djeca”. Zato dajem sve od sebe da improviziram, kao kad sam mu napravio sendviče s jabukama. Ponekad druga djec
 Bakterije u rodnom kanalu povezane su s manjim rizikom od raka jajnika
Nova studija pokazuje da nešto tako jednostavno kao što je bris cerviksa može imati potencijal pomoći stotinama žena koje su u iznimno velikom riziku od raka jajnika jer imaju mutaciju u genu BRCA1.
Bakterije u rodnom kanalu povezane su s manjim rizikom od raka jajnika
Nova studija pokazuje da nešto tako jednostavno kao što je bris cerviksa može imati potencijal pomoći stotinama žena koje su u iznimno velikom riziku od raka jajnika jer imaju mutaciju u genu BRCA1.