 Hvad er HCV, hvordan overføres det, er der symptomer, og kan det helbredes?
Hvad er HCV, hvordan overføres det, er der symptomer, og kan det helbredes?De fleste mennesker, der får hepatitis C (hep C), har ingen symptomer. De, der har symptomer, kan dog opleve:
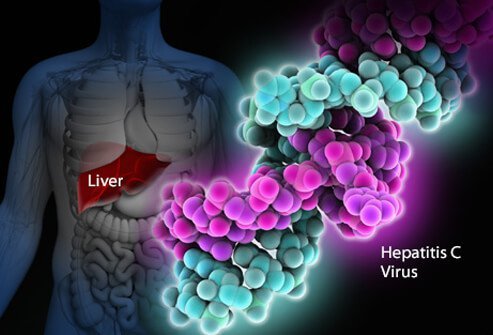
Hepatitis C-virusinfektion er en infektion i leveren forårsaget af hepatitis C-virus (også kaldet HCV eller hep C). Det er svært for det menneskelige immunsystem at fjerne hepatitis C fra kroppen, og infektion med hepatitis C bliver normalt kronisk. Gennem årtier skader kronisk infektion med hepatitis C leveren og kan forårsage leversvigt. I USA har CDC anslået, at cirka 41.200 nye tilfælde af hepatitis C opstod i 2016. Når virussen først kommer ind i kroppen, er der normalt ingen symptomer, så dette tal er et skøn. Omkring 75%-85% af nysmittede mennesker bliver kronisk inficerede. I USA anslås mere end 2 millioner mennesker at være kronisk inficeret med hepatitis C. Infektion opdages oftest blandt mennesker i alderen 40 til 60 år, hvilket afspejler de høje infektionsrater i 1970'erne og 1980'erne. Der er 8.000 til 10.000 dødsfald hvert år i USA relateret til hepatitis C-infektion. HCV-infektion er den førende årsag til levertransplantation i USA og er en risikofaktor for leverkræft. I 2016 angav 18.153 dødsattester HCV som en medvirkende dødsårsag; dette menes at være en undervurdering.
Omkring 10%-20% af dem, der udvikler kronisk HCV, vil udvikle cirrose inden for 20-30 år. Progression til skrumpelever kan accelereres af alder over 50, mandligt køn, alkoholforbrug, ikke-alkoholisk fedtleversygdom (NASH), samtidig infektion med hepatitis B eller HIV og immunundertrykkende stoffer. HCV-infektion er den førende årsag til levertransplantation på grund af leversvigt i USA.
De, der har cirrhose fra HCV, har også en årlig risiko for leverkræft (hepatom eller hepatocellulært carcinom) på omkring 1%-5%.
Hepatitis betyder betændelse i leveren. Hepatitis C er en af flere vira, der kan forårsage viral hepatitis. Det er ikke relateret til de andre almindelige hepatitisvirus (for eksempel hepatitis A eller hepatitis B). Hepatitis C er et medlem af Flaviviridae familie af virus. Andre medlemmer af denne familie af vira omfatter dem, der forårsager gul feber og denguefeber.
Der er mindst seks forskellige genotyper (stammer) af virussen, som har forskellige genetiske profiler (genotype 1 til 6). I USA er genotype 1 den mest almindelige stamme af hepatitis C. Selv inden for en enkelt genotype kan der være nogle variationer (f.eks. genotype 1a og 1b). Genotyping bruges til at vejlede behandling, fordi nogle virale genotyper reagerer bedre på nogle terapier end på andre.
Ligesom human immundefektvirus (HIV) formerer hepatitis C sig meget hurtigt og opnår meget høje niveauer i kroppen. De gener, der får virusets overfladeproteiner til at mutere (ændres) også hurtigt, og tusindvis af genetiske variationer af virussen ("kvasi-arter") produceres dagligt. Det er umuligt for kroppen at holde trit med at lave anti-HCV-antistoffer mod alle de kvasi-arter, der cirkulerer på én gang. Det har endnu ikke været muligt at udvikle en effektiv vaccine, fordi vaccinen skal beskytte mod alle genotyper.
Hepatitis C-infektion i leveren udløser immunsystemet, hvilket fører til betændelse. Omkring 20%-30% af de akut inficerede vil opleve typiske hepatitissymptomer såsom mavesmerter, gulsot, mørk urin eller lerfarvet afføring. Men kronisk hepatitis C forårsager normalt ingen symptomer før meget sent i sygdommen, og hepatitis C er blevet omtalt af syge som den "sovende drage". Over flere år eller årtier kan kronisk inflammation forårsage levercellers død og ardannelse ("fibrose"). Omfattende ardannelse i leveren kaldes skrumpelever. Dette forringer gradvist leverens vitale funktioner. Skrumplelever er mere tilbøjelige til at få leverkræft. At drikke alkohol fremskynder leverskader med hepatitis C. Samtidig HIV-infektion såvel som akut hepatitis A- eller B-infektion vil også fremskynde progression til skrumpelever.
Omkring 70%-80% af mennesker har ingen symptomer, når de først får HCV-infektion. De resterende 20%-30% kan have
Tidlige symptomer på hepatitis C kan omfatte mørk urin, gule øjne eller lerfarvet afføring, selvom dette er usædvanligt. Over tid kan personer med kronisk HCV-infektion udvikle tegn på leverbetændelse, der tyder på, at infektionen kan være til stede. Inficerede individer kan let blive trætte eller klage over uspecifikke symptomer. De senere symptomer og tegn på skrumpelever er ofte fraværende, indtil betændelsen er ret fremskreden. Efterhånden som skrumpelever skrider frem, øges symptomer og tegn og kan omfatte:
Fordi hepatitis C overføres ved eksponering for blod, er der ingen specifik periode med smitsomhed. Mennesker, der udvikler kronisk hepatitis C, bærer virussen i deres blod og smitter derfor af andre hele deres liv, medmindre de er helbredt for deres hepatitis C.
Det er svært at sige med sikkerhed, hvad inkubationstiden for hepatitis C er, fordi de fleste mennesker, der er smittet med hepatitis C, ikke har symptomer tidligt i infektionsforløbet. De, der udvikler symptomer tidligt efter at være blevet smittet (i gennemsnit 2 til 12 uger, men kan være længere), oplever milde gastrointestinale symptomer, som måske ikke beder om et besøg hos lægen.
De fleste af tegnene og symptomerne på hepatitis C-infektion relaterer sig til leveren. Sjældnere kan hepatitis C-infektion påvirke andre organer end leveren.
Hepatitis C-infektion kan få kroppen til at producere unormale antistoffer kaldet kryoglobuliner. Kryoglobuliner forårsager betændelse i arterierne (vaskulitis). Dette kan beskadige hud, led og nyrer. Patienter med kryoglobulinæmi (kryoglobuliner i blodet) kan have
Derudover kan inficerede individer med kryoglobulinæmi udvikle Raynauds fænomen, hvor fingre og tæer skifter farve (hvide, så lilla, så røde) og bliver smertefulde ved kolde temperaturer.
U.S. Preventive Health Services-taskforcen anbefaler, at alle voksne født mellem 1945 og 1965 testes én gang rutinemæssigt for hepatitis C, uanset om risikofaktorer for hepatitis C er til stede. Engangstest anbefales også til:
Personer, der kan have været udsat for hepatitis C i de foregående 6 måneder, bør testes for viral RNA-belastning i stedet for anti-HCV-antistof, fordi antistof muligvis ikke er til stede i op til 12 uger eller længere efter infektion, selvom HCV-RNA kan påvises i blodet så hurtigt som 2-3 uger efter infektion.
Generelt kan årlig screening være passende for personer med vedvarende risikofaktorer såsom gentagne seksuelt overførte sygdomme (STD'er) eller mange sexpartnere, igangværende intravenøs stofbrug eller langvarige sexpartnere for personer med hepatitis C. Hvorvidt der skal testes eller ej. disse personer bestemmes ud fra en sag til sag.
Der er en 4%-7% risiko for at overføre HCV fra mor til spædbarn ved hver graviditet. I øjeblikket er der ingen CDC-anbefaling for rutinemæssig hepatitis C-screening under graviditet, og der er ingen i øjeblikket anbefalet medicin til at forhindre overførsel fra mor til spædbarn (profylakse). CDC overvåger dog forskningsresultater og kan komme med anbefalinger i fremtiden, efterhånden som der opstår beviser.
Mens data stadig er begrænsede, fandt en nylig undersøgelse af over 1.000 tilfælde i Det Forenede Kongerige, at 11 % af spædbørn var blevet smittet ved fødslen, og at disse spædbørn sandsynligvis udviklede skrumpelever i deres tidlige 30'ere. Sagen for screening for HCV under graviditet omfatter potentialet for sikkert at behandle mødre under graviditeten med direkte virkende antivirale midler (DAA'er) til at behandle moderen før skrumpelever udvikler sig, forhindre spædbarnsoverførsel og forhindre overførsel til andre. Børn født af HCV-inficerede mødre kan også tilbydes behandling i en tidlig alder for at forhindre skrumpelever samt overførsel til andre. Koordinering af pleje mellem flere specialister vil være vigtig for at nå disse mål.
Børn af HCV-inficerede mødre kan screenes for hepatitis C så tidligt som i 1-2 måneders alderen ved hjælp af hepatitis C viral load eller PCR-test (se Blodprøver for hepatitis C). Antistoffer mod hepatitis C, som overføres fra mor til barn, vil være til stede i op til 18 måneder, så børn bør tidligst testes for HCV-antistof.
Hepatitis C behandles af enten en gastroenterolog, en hepatolog (en gastroenterolog med yderligere uddannelse i leversygdom) eller en infektionssygdomsspecialist. Behandlingsteamet kan omfatte mere end én specialist, afhængigt af omfanget af leverskader. Kirurger, der er specialiserede i kirurgi af leveren, herunder levertransplantation, er en del af det medicinske team og bør se patienter med fremskreden sygdom (leversvigt eller skrumpelever) tidligt, før patienten skal have en levertransplantation. De kan muligvis identificere problemer, der skal løses, før operation kan overvejes. Andre personer, der kan være behjælpelige med at håndtere patienter, omfatter diætister til at rådføre sig om ernæringsmæssige spørgsmål og farmaceuter til at hjælpe med behandling af lægemidler.
Der er flere blodprøver til diagnosticering af hepatitis C-infektion. Blod kan testes for antistof mod hepatitis C (anti-HCV antistof). Det tager omkring 8-12 uger i gennemsnit og op til 6 måneder for antistoffer at udvikle sig efter den første infektion med hepatitis C, så screening for antistoffer kan gå glip af et par nyligt inficerede individer. At have antistoffer er ikke en absolut indikation af aktivt, multiplicerende hepatitis C-virus, men hvis antistoftesten er positiv (antistof er til stede), er den statistiske sandsynlighed for aktiv infektion større end 99 %.
Adskillige tests er tilgængelige for at måle mængden af hepatitis C-virus i en persons blod (virusmængden). Hepatitis C-virusets RNA kan identificeres ved en type test kaldet polymerasekædereaktion (PCR), der detekterer cirkulerende virus i blodet allerede 2-3 uger efter infektion, så det kan bruges til at opdage formodet akut infektion med hepatitis C tidlig infektion. Det bruges også til at bestemme, om aktiv hepatitis er til stede hos en person, der har antistoffer mod hepatitis C, og til at følge virusbelastningen under behandlingen.
Blodprøver udføres også for at identificere genotyperne af HCV. Genotyper reagerer forskelligt på forskellig behandling, så denne information er vigtig ved udvælgelsen af det mest passende behandlingsregime.
Estimering af leverfibrose ved hjælp af blodprøver er også ret pålidelige til diagnosticering af klinisk signifikant ardannelse; disse omfatter FIB-4, FibroSure, Fibrotest og aspartat aminotransferase-til-blodplade-forholdsindeks (APRI).
Det næste trin er at bestemme niveauet af leverardannelse, der er opstået. Leverbiopsi tillader undersøgelse af en lille prøve af levervæv under et mikroskop, men leverbiopsi er en invasiv test og har betydelige risikoer for blødning. Det kan også savne unormale områder i tidlig sygdom.
Ikke-invasive tests har stort set erstattet leverbiopsi undtagen i særlige situationer. Leverstivhed indikerer, at fremskreden leverardannelse eller skrumpelever kan være til stede. Transient elastografi kan bruges til at måle denne stivhed ved hjælp af ultralyd eller magnetisk resonansbilleddannelse (MRI).
Evaluering før behandling for hepatitis C bør også omfatte:
Interferons, for example, Roferon-A and Infergen, and pegylated interferons such as Peg-Intron T , Pegasys, were mainstays of treatment for years. Interferons produced sustained viral response (SVR, or cure) of up to 15%. Later, peglatedll forms produced SVR of 50%-80%. These drugs were injected, had many adverse effects, required frequent monitoring, and were often combined with oral ribavirin, which caused anemia. Treatment durations ranged up to 48 weeks.
Direct-acting anti-viral agents (DAAs) are antiviral drugs that act directly on hepatitis C multiplication.
Hepatitis C treatment is best discussed with a doctor or specialist familiar with current and developing options as this field is changing, and even major guidelines may become outdated quickly.
The latest treatment guidelines by the American Association for the Study of Liver Disease (AASLD) and Infectious Disease Society of America (IDSA) recommends use of DAAs as first-line treatment for hepatitis C infection. The choice of DAA varies by specific virus genotype, and the presence or absence of cirrhosis. In the U.S., specific insurance providers also might influence the choice due to the high cost of DAAs. Although the individual, public health, and cost benefits of treating all patients with hepatitis C is clear, the most difficult barrier to treating all people with HCV is the very high cost of the drug regimens. Patients are encouraged to discuss options with their health care professional.
Treatment is recommended in all patients with chronic hepatitis C unless they have a short life expectancy that is not related to liver disease. Severe life-threatening liver disease may require liver transplantation. Newer therapies with DAAs have allowed more and more patients to be treated.
The ultimate goals of antiviral therapy are to
A side goal is preventing co-infections with other hepatitis viruses, such as A and B, which can cause more liver disease than HCV alone. These can be prevented by vaccines and treatment.
When people first get hepatitis C, the infection is said to be acute. Most people with acute hepatitis C do not have symptoms so they are not recognized as being infected. However, some have low-grade fever, fatigue or other symptoms that lead to an early diagnosis. Others who become infected and have a known exposure to an infected source, such as a needlestick injury, are monitored closely.
Treatment decisions should be made on a case-by-case basis. Response to treatment is higher in acute hepatitis infection than chronic infection. However, many experts prefer to hold off treatment for 8-12 weeks to see whether the patient naturally eliminates the virus without treatment. Approaches to treatment are evolving. Patients with acute hepatitis C infection should discuss treatment options with a health care professional who is experienced in treating the disease. There is no established treatment regimen at this time.
If the hepatitis C RNA remains undetectable at the end of the treatment and follow-up period, this is called a sustained virologic response (SVR) and is considered a cure. Over 90% of people treated with DAAs are cured. These people have significantly reduced liver inflammation, and liver scarring may even be reversed.
About 5% of people who are treated for HCV infection are not cured by some of the older regimens. These people may still have options for cure with the newer regimens.
Few people with hepatitis C are at risk for problems if they are treated, however there are some factors that affect treatment regimens, such as concurrent HIV medications and kidney dysfunction. Some drugs are not safe for people with cirrhosis. Individuals who are unable to comply with the treatment schedule for psychological reasons or ongoing drug or alcohol abuse may not be good candidates for treatment because the drugs are very costly and require adherence to the pill regimen and regular follow-up visits. There are some important drug interactions with some of the medications that should be considered by the health care professional.
People with past hepatitis B or who have chronic active hepatitis B should not be treated for HCV without treating for HBV as well. As highly effective treatment for HCV has emerged, reports of serious hepatitis B have come to light. Similar to HCV, hepatitis B usually does not clear from the liver after acute infection, even though it is far less likely to cause chronic active hepatitis than hepatitis C infection. It remains dormant in most people, but it can reactivate with changes in the immune system. It is not clear why eliminating the HCV can allow the HBV infection to flare up. Hepatitis B screening is an important part of the hepatitis C evaluation. Those who have laboratory evidence of active or past infection with HBV should be monitored while receiving HCV treatment.
Compared to interferons and ribavirin drugs, the side effects of DAAs are far fewer and more tolerable. These side effects usually do not require discontinuation of therapy and are self-limiting after completion of therapy.
Patients with hepatitis B co-infection should be monitored for symptoms of reactivation of hepatitis, which are the same as the symptoms of acute hepatitis. The treating doctor may perform blood screening for this as well.
Hepatitis C is the leading reason for 40% to 45% of liver transplants in the U.S. Hepatitis C usually recurs after transplantation and infects the new liver. Approximately 25% of these patients with recurrent hepatitis will develop cirrhosis within five years of transplantation. Despite this, the five-year survival rate for patients with hepatitis C is similar to that of patients who are transplanted for other types of liver disease.
Most transplant centers delay therapy until recurrent hepatitis C in the transplanted liver is confirmed. Oral, highly effective, direct-acting antivirals have shown encouraging results in patients who have undergone liver transplantation for hepatitis C infection and have recurrent hepatitis C. The choice of therapy needs to be individualized and is rapidly evolving.
Once patients successfully complete treatment, the viral load after treatment determines if there is an SVR or cure. If cure is achieved (undetectable viral load after treatment), no further additional testing is recommended unless the patient has cirrhosis. Those who are not cured will need continued monitoring for progression of liver disease and its complications.
While cure eliminates worsening of fibrosis by hepatitis C, complications may still affect those with cirrhosis. These individuals still need regular screening for liver cancer as well as monitoring for esophageal varices that may bleed.
Because hepatitis B co-infection may reactivate or worsen even after treatment for HCV, monitoring for hepatitis symptoms may be needed after the end of therapy.
At this time there are no effective home or over-the-counter treatments for hepatitis C.
Over several years or decades, chronic inflammation may cause death of liver cells and cirrhosis (scaring, fibrosis). When the liver becomes cirrhotic, it becomes stiff, and it cannot perform its normal functions of clearing waste products from the blood. As fibrosis worsens, symptoms of liver failure begin to appear. This is called "decompensated cirrhosis " or "end-stage liver disease. " Symptoms of end-stage liver disease include:
The liver and spleen have an important function of clearing bacteria from the blood stream. Cirrhosis affects many areas of immune function, including attraction of white blood cells to bacteria, reduced killing of bacteria, reduced production of proteins involved in immune defenses, and decreased life span of white blood cells involved in immune defenses. This may be referred to as having cirrhosis-associated immune dysfunction syndrome or CAIDS.
Transmission of hepatitis C can be prevented in several ways.
Prevention programs aim at needle sharing among drug addicts. Needle exchange programs and education have reduced transmission of hepatitis C infection. However, IV drug users are a difficult to reach population, and rates of hepatitis C remain high among them.
Among health care workers, safe needle-usage techniques have been developed to reduce accidental needlesticks. Newer needle systems prevent manual recapping of needles after use of syringes, which is a frequent cause of accidental needlesticks
There is no clear way to prevent hepatitis C transmission from mother to fetus at this time.
People with multiple sexual partners should use barrier precautions such as condoms to limit the risk of hepatitis C and other sexually transmitted diseases, including HIV.
If one partner is infected, monogamous couples may want to consider the low risk of transmission of hepatitis C infection when deciding whether to use condoms during sex. Some couples may decide to use them and some may not.
Screening of the blood supply has almost eliminated the risk of transmission of hepatitis C infection through transfusion.
People with hepatitis C infection should not share razors or toothbrushes with others because of the possibility that these items may be contaminated with blood.
People who want to get a body piercing(s) or tattoo(s) are encouraged to do so only at licensed piercing and tattoo shops (facilities), and verify that the body piercing or tattoo shop uses infection-control practices.
It is critical that physicians and clinics follow manufacturers and regulatory agency directions for sterilizing/cleaning instruments and that disposable instruments be discarded properly. There is no need to use special isolation procedures when dealing with hepatitis C infected patients.
In general, among patients with untreated hepatitis C:
Drinking alcohol and acquiring other hepatitis viruses are risk factors for worse liver disease. People with chronic hepatitis C should avoid drinking alcohol and should be screened for antibodies to hepatitis A and B. If they do not have antibodies, they should be vaccinated against these other hepatitis viruses.
People with hepatitis C should be educated about preventing HIV infection. Infection with both HIV and hepatitis C speeds up and worsens liver damage caused by hepatitis C. Hepatitis C also can affect the HIV infection and how it is treated. About 25% of people with HIV infection are co-infected (also infected) with hepatitis C, and up to 90% of IV drug users with HIV are co-infected with hepatitis C. Screening for hepatitis viruses is important in all people infected with HIV, just as screening for HIV is important in people who have hepatitis C.
Liver cancer (hepatocellular carcinoma, or hepatoma) is associated with cirrhosis from chronic hepatitis C. Some experts recommend screening patients with hepatitis C infection and cirrhosis for liver cancer periodically.
As our knowledge of hepatitis C increases, more and more patients are being diagnosed with chronic infection. Current research is very active and includes diagnosis, natural history, treatment, and vaccine development. Thus the field is constantly changing, with new guidelines added frequently.
 Stigende risiko for bioforsvar ved syntetisk biologi
En undersøgelse fra et amerikansk forsvarsministerium har fundet ud af, at der er flere gentekniske værktøjer, der kan bruges til at udforme biologiske våben på kort tid. Den omfattende rapport på 2
Stigende risiko for bioforsvar ved syntetisk biologi
En undersøgelse fra et amerikansk forsvarsministerium har fundet ud af, at der er flere gentekniske værktøjer, der kan bruges til at udforme biologiske våben på kort tid. Den omfattende rapport på 2
 Hvor alvorlig er Crohns sygdom?
Hvad er Crohns sygdom? Crohns sygdom i sig selv er normalt ikke livstruende, selvom den kan forårsage alvorlige eller dødelige komplikationer, som omfatter tarmobstruktion, fistler, analfissurer og
Hvor alvorlig er Crohns sygdom?
Hvad er Crohns sygdom? Crohns sygdom i sig selv er normalt ikke livstruende, selvom den kan forårsage alvorlige eller dødelige komplikationer, som omfatter tarmobstruktion, fistler, analfissurer og
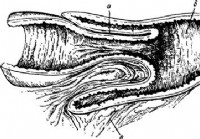 Ufremkommelighed fra implementering af tarme - Diagnose af akut abdomen
Implementering eller vdviganiye af et stykke tarm i et andet som årsagen til tarmens ufremkommelighed, observeres ikke i alle lande med en identisk frekvens. På store engelske statistikker (London, 19
Ufremkommelighed fra implementering af tarme - Diagnose af akut abdomen
Implementering eller vdviganiye af et stykke tarm i et andet som årsagen til tarmens ufremkommelighed, observeres ikke i alle lande med en identisk frekvens. På store engelske statistikker (London, 19